Overview
A key driver on the path to value-based care involves Primary Care Providers (PCPs) accepting more responsibility for the health of their patients. When presented with the opportunity to steer patients to higher performing specialty care (and, of course, when practical), PCPs can drive utilization to providers that not only manage costs and outcomes more effectively, but also benefit patients in the long run.
Physician-Patient Relationship
Think of a PCP as a pilot, with patients as the passengers. Patients count on their PCP to manage their health, guide them, and get them from Point A to Point B (or from diagnosis to treatment) safely. The role of the PCP – who can be an internist, general practitioner, nurse practitioner, or physician assistant – is to serve as a jack-of-all-trades. In some instances, the PCP may need a “co-pilot” and rely on specialists to diagnose a condition, determine an appropriate treatment plan, or simply offer an expert’s opinion, given that specialists can hone in on the specific branch of medicine in which they were trained.
As value-based care adoption grows, PCPs are increasingly accountable (and incentivized) for more of the total cost and quality of care delivered to patients assigned to them (or attributed to the PCP). Providers that administer higher quality, lower cost care are paid more by payers like CMS, while those who deliver lower quality and/or more expensive care are paid less. In some cases, PCPs may also be responsible for care rendered by other providers to patients who are still attributed to that PCP. Additionally, PCPs are “beginning to understand the cost implications of their decisions [on] patients, as more patients face rising out-of-pocket costs, like coinsurance, copays, and higher deductibles.”
With PCPs in the driver’s seat, they have the opportunity to route patients to specialty care that is mutually beneficial for the PCP and the patient. The cost and quality of a patient’s specialty care can be the difference between a smooth ride or one brimming with turbulence.
Data: Just What the Doctor Ordered
In 2018, a survey of 624 PCPs and specialty physicians was conducted and representative of the American Medical Association Masterfile in terms of years in practice, gender, geography, practice type, and specialty. The survey revealed that while two-thirds of the physicians received some quality and productivity information, the vast majority (72%) did not receive cost information. The study found physicians did not receive cost or resource use for their attributed patients, for physicians and facilities to which they refer, nor did they receive estimated patient out-of-pocket costs. Additionally, physicians who did receive cost data for physicians and facilities to which they refer indicated that this knowledge changed their behavior and the way they referred patients. Respondents also shared that data on healthcare costs allowed them to feel better prepared to participate in value-based payment models and deliver better outcomes while managing resources.
In the past, referrals were handled through a professional network, with specialists meeting internist and family doctors at hospitals, conferences, medical school alumni meetups, and even the occasional golf club. Of course, many referrals were still informed by a provider’s credentials and ability to help their patients. Today, many industry and networking events have moved online, and doctors and patients alike have a dizzying array of specialists to choose from. When PCPs no longer rely on their rolodex to remember the name of a “good” specialist, data is key to identifying a specialist that would be in their patient’s best clinical and financial interests.
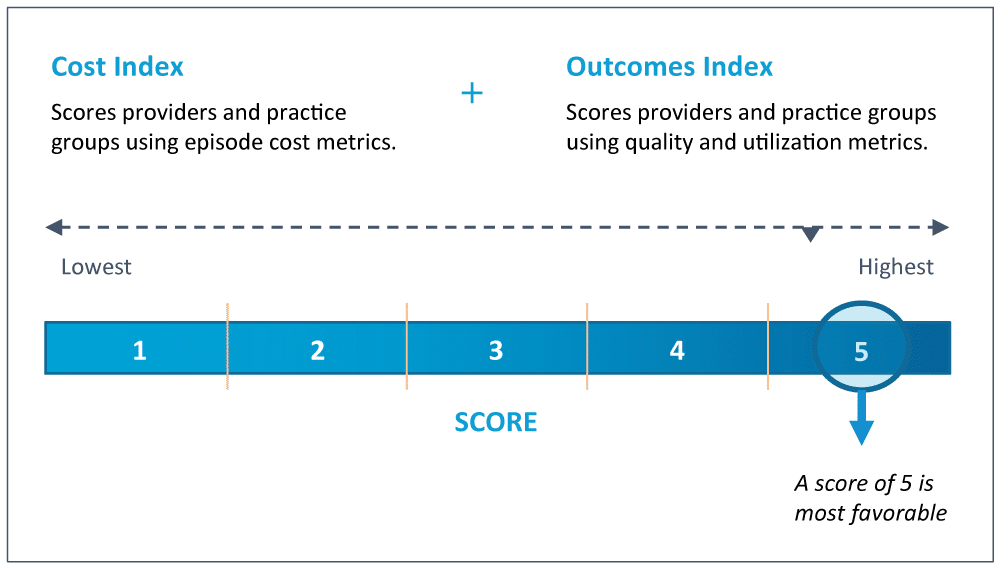
CareJourney’s Provider Performance Index (PPI) offers a reliable and transparent scoring system to evaluate the cost and quality of PCPs and specialists. The two scores (one for cost, one for outcomes) are risk-adjusted, benchmarked regionally, and inclusive of a provider’s taxonomy (or sub-specialty). In other words, the PPI measures what matters most and is powered by the following features:
- Robust, Longitudinal Data – Scores are built using 100% Medicare claims data to create a comprehensive view of a patient’s journey, which directly contributes to a provider’s performance.
- Open Methodologies – Cost and quality are aggregated using open methodologies pioneered by CMS.
- Trusted Enrichments – The PPI assesses quality using industry-accepted definitions of low value, avoidable, and/or appropriate care.
Providers and their organizations can use the PPI to understand their ability to manage the cost and quality of their patient outcomes, as well as the PPI scores of specialists to whom they are referring or that are already being utilized by their patients to better inform their specialist recommendations.
How Provider Performance Data Can Improve Referrals
In this example, see how referrals to higher performing cardiologists result in potential savings of over $3k per episode.
How CareJourney Can Help
With access to the complete Medicare FFS dataset, information on providers both in and out of your network, and a breakdown of episodes contributing to PPI Cost and Outcomes Scores, CareJourney analytics can help:
- Identify where patients in your primary care network are utilizing specialty care by individual provider, practice group, or ACO level nationally and in your geographic region
- Determine which providers are delivering high value, low cost specialty care (and those who are not and why)
- Assess which PCPs are affiliated with patients that are receiving care from high value specialists already in your network
- Provide additional cost and utilization metrics for comparison
If you want to better understand how CareJourney can help you gain insights into higher performing specialty care, please email us at jumpstart@carejourney.com, request a meeting at the link below, or explore our other resources to get a sense of how CareJourney supports organizations involved in (or on the path to) value-based care through data analytics.
