The Challenge of Benchmarking Provider Performance
It is critical for health care organizations to find novel ways to engage providers to help improve quality, reduce the cost of care, and track progress. Finding data that helps benchmark provider performance in these areas is not difficult, however, the models used in most rating systems today are opaque and have not garnered much adoption from the industry. You can spend a lot of time and money on crunching data using proprietary models and end up with metrics that you cannot trust, nor verify. The challenge is the absence of a single, reliable, and transparent way to measure provider performance that can be used as an industry standard for making critical decisions.
Introducing CareJourney’s Provider Performance Index
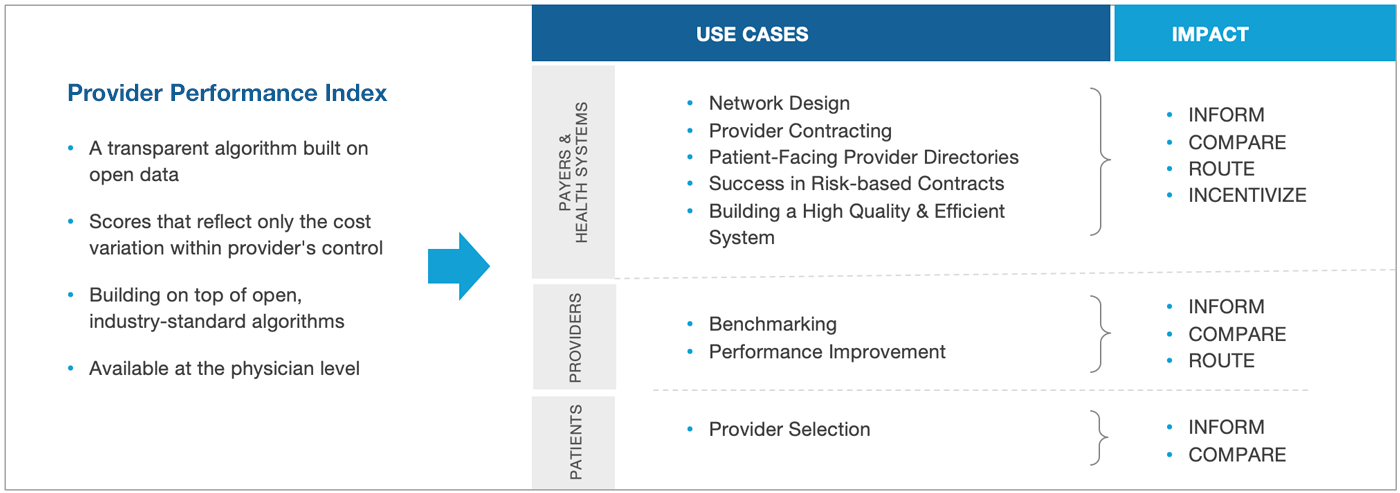
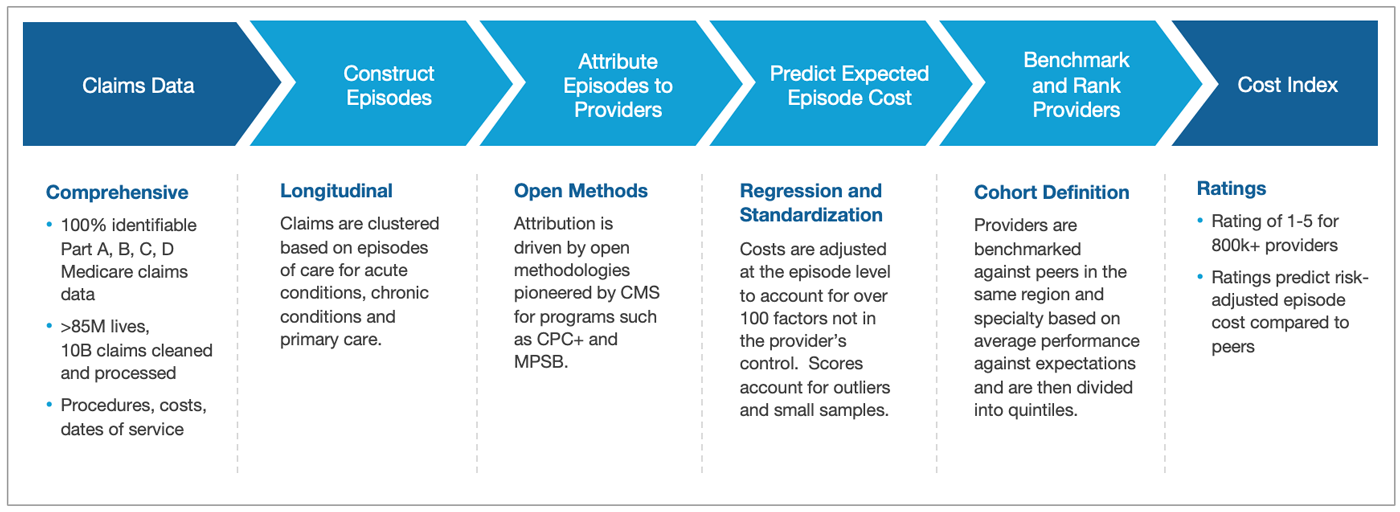
CareJourney did a rigorous analysis of the most successful open methodologies and developed a reliable way to measure and track provider performance across over 800,000 providers, including Primary Care Physicians (PCPs) and Specialists, across dozens of industry-accepted cost and outcome metrics using easy-to-understand Cost and Outcome scores.
A Breakthrough in Measuring Provider Performance. No Black Boxes.
Our Index allows you to run quick comparisons of provider cost efficiency and quality outcomes by allowing you to model provider accountability based on patient episodes, instead of individual treatments or procedures. By analyzing risk-adjusted cost performance and combining over 20 different outcomes metrics, we’ve developed a simple and easy way to stratify providers into high or low performing categories on either their cost or quality score for any region in the country. This saves valuable time and side-steps additional costly analysis required to analyze episodic costs and quality measures across disparate data points.
Measure What Matters
The Provider Performance Index scores PCPs and Specialists on two five-point scales, one for Cost and one for Outcomes, corresponding to quintiles of performance against similar providers in their region. Our approach has unlocked a novel way to leverage already-accepted metrics, building on standard component algorithms for attribution, risk adjustment, and episode bundling, thereby making them auditable and comprehensive.
“Our current indicators for measuring network performance against competitors are inadequate because they only use Per Member Per Year (PMPY) costs, which is meaningless without the observed vs expected adjustments. Additionally, we struggle with attributing dollars to specialists since they are not responsible for the total cost of care. The Provider Performance Index effectively solves both problems because it normalizes scores and compares providers that treat similar populations. It also takes an episodic approach based on the MSPB metric, which is much more meaningful for specialists.”
Network Operations Director
Major Health Care Management Company
Make Data-informed Decisions
The CareJourney Index allows multiple actors in the healthcare industry to compare providers using a universal scoring system.
|
Payers
|
|
|
Health Systems
|
|
|
Physicians
|