By Jackie Beltejar
The Data Conundrum
The past decade has seen a remarkable increase in the number of lives covered in risk-based contracts. According to a recent article by Leavitt Partners published in Health Affairs, “At the end of the first quarter of 2018, we were tracking a total of 1,011 ACOs representing 1,477 distinct active accountable care payment contracts with public and private payers. Combined, these contracts cover about 32.7 million patients in all regions of the country”.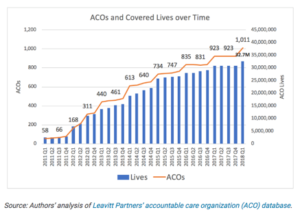
Accountable care organizations (ACOs) and other risk-bearing entities are faced with hard decisions everyday as healthcare leaders are put under increasing pressure to optimize their networks in order to lower costs and improve outcomes. Many organizations lack the tools to do so, let alone know where to begin.
This blog illustrates the approach that one of our members has taken to leverage the vast depth and breadth of data and insights that are offered through our Network Advantage and Populations Insights products and made significant improvements to their networks, in their journey towards value-based care.
A Strategic Approach to Tackling Organization-wide Challenges Using Claims Data
Our member, an integrated delivery system, comprised of over 350 facilities and 87,000 employees servicing 2.6 million patients per year, has developed a technique that threads together two of CareJourney’s data platforms to build and optimize their provider networks across their ACOs.
Identifying Market Expansion Opportunities
The first phase of work pulls from Network Advantage, our analytics platform which contains the full Medicare fee-for-service claims dataset (65 million Americans) over eight years and updated quarterly. The member uses this tool to first identify opportunities for market expansion in geographical regions of the country they are currently operating in. The platform is their window into more than just their network’s data, but the full breadth of data on every provider nationwide. Using this tool, the member can gather information on how their in-network providers are interacting with out-of-network entities. Additionally, they used this platform to evaluate high-performing providers and practice groups they may want to consider working with. With this data, they’ve approached several practice groups and have successfully expanded their network into other states.
Build and Optimize Networks of Care with Network Advantage
REQUEST A DEMO
Tracking Longitudinal Performance and Improve Network Management
The second phase of work taps into our Population Insights platform which drills down into claim-level data of the risk-bearing entity. Via this platform, the user can track the longitudinal performance of their previous network and newly established network, side by side. A few key performance metrics that have served valuable to this member are expenditures by component (e.g., inpatient, outpatient, skilled nursing facility, home health, etc.) and total per member per year spend over time to help them understand spending trends, as well as dashboards that hone in on annual wellness visits and transitional care management performance to identify areas where they can prevent unnecessary spend and achieve cost savings. Armed with this data, they can work with providers on areas of improvement and continuously track their efforts over time.
Additionally, they have recognized that to be a successful organization, they have to be truly physician-led because it’s the physicians that know their patients best. The member has taken this philosophy and proven it by adopting a physician-prescribed patient segmentation model into their workflows to help providers manage their patients. In partnership with CareJourney, they can now access a list of patients that they consider ‘high risk’ — based on a single provider’s local understanding of the patient cohorts in the region he practices — and apply the appropriate clinical intervention. This homegrown patient segmentation model is just one example of how CareJourney has sourced care models from clinical leaders; we can expect more of these in the future as data becomes more readily available at the point of care.
Securing Network Integrity
Finally, the third phase involves fostering relationships with providers in the community to earn a spot as a “preferred provider”. One area of concern within the organization was weak referral systems whereby their patients were going to out of network facilities to receive care. The member collaborated with CareJourney to develop a claims-based algorithm, which goes beyond co-occurrence of claims between providers, to better understand and track the extent of the problem. They developed a targeted strategy to improve network integrity. The member has just begun taking steps to improve their referral management systems by leveraging data from Network Advantage to create 1-pagers for their physician liaisons to take into meetings with providers. These physician liaisons use the data as a guide to begin the conversation to see if there’s potential to be a “preferred partner” in the community. Using Network Advantage, they can continue to track referral patterns over time to understand how efficient their network is operating with the end goal of optimizing network integrity across the continuum of care.
The availability of usable, actionable data has given ACO’s and other risk bearing entities new ground to stand on, one where they can make informed decisions backed by their own data. By organizing data in a way that makes sense, leaders are equipped with the necessary information they need to make strategic decisions.
What’s next?
As we continue to build out our analytical capabilities in response to industry-wide challenges, members can expect to see new features that help them understand referral patterns of primary care providers to specialists, specialists to specialists, and provider (primary or specialist) to institutional facilities. This will allow for greater transparency into referral behavior among their providers and increase their ability to identify critical opportunities for network expansion.
At CareJourney, we value a collaborative approach to product development, which is largely driven by the end user. The healthcare system is continuously changing year by year. For that reason, technology and healthcare cannot afford to operate in silos any longer. We honor an open-source, non-black box approach to data analytics which allows users to understand our methodologies, critique it, and lend their insights into ways we can improve upon it. We look to industry leaders across technology, healthcare, and government to influence the way we envision and build our products to ensure we are building analytical capabilities that are keeping up with the changing healthcare landscape.
Build and Optimize Networks of Care with Network Advantage
REQUEST A DEMOMember Spotlight: Webinar on 10/15, 1-2PM ET
Universal Health Systems (UHS) Case Study: How to Improve Network Design and Management with Claims Data. Sign up for this webinar today!
