Blue Button 2.0: Everything You Need to Know and More!
Joe Mercado
December 14, 2020
Request Meeting
Overview & Brief History of Blue Button
Blue Button is an initiative established by the Centers for Medicare & Medicaid Services (CMS) and the Veteran’s Administration (VA) in 2010. The original program laid the groundwork for Blue Button 2.0 as we know it today. Blue Button is a movement toward an improved healthcare system in which patients and providers use information technology and all available data points to collaborate and improve a patient’s health.
Today’s manifestation of Blue Button is a standards-based application programming interface (API) that delivers Medicare claims history (Part A, B, and D data) for over 60 million Medicare beneficiaries from May 2014 to present.1 Blue Button 2.0 has been used by more than 1 million Medicare beneficiaries to download their CMS claims history via the MyMedicare.gov portal, essentially creating a chronology of all their medical procedures, diagnoses, and more.
Using these extensive claims data points, various healthcare entities can1:
- Reduce patient burden
- Streamline information about different kinds of care over time
- Uncover new insights that can improve health outcomes
- Access and monitor health information in one place
Why Understanding Risk Scoring in the ACO REACH Model is Critical For Success
One major concern about the Direct Contracting model was risk scoring abuse. Read how the updated model plans to address risk scoring.
Blue Button 2.0 is a Fast Healthcare Interoperability Resource (FHIR)-based claims API for Medicare beneficiaries. This means that it delivers patient claims information in a secure, standard way. Blue Button 2.0, originates from the MyHealthEData program established in 2018 and provides beneficiaries the ability to procure their claims history and also securely connect their claims data to apps and other tools made available to them. As of December 2020, over 60 organizations have Blue Button apps available and over 2,500 developers are working on development of applications.2
While there is significantly more work to be done, CMS has been successful with their goal of creating a “developer-friendly, standards-based data API that enables beneficiaries to connect their Medicare claims data to the applications, services, and research programs they trust.”3
CareJourney is especially excited about the strides made around Blue Button because of the implications for:
Voluntary Alignment: A key component to the Direct Contracting Program, Direct Contracting Entities’ (DCE) fee-for-service providers can get insight into their beneficiaries through Blue Button claims as part of the DCE, as early as during a patient recruiting process. Historical claims data will provide insight into the needs of the patient population to ensure DCEs are adequately staffed to support the beneficiary’s current and future needs.
MA Switchers/Risk Adjustment: Organizations can gain insight into the potential beneficiaries switching from traditional Fee-For-Service into a Medicare Advantage (MA) plan. Specifically, Blue Button can provide MA plans with a beneficiary’s historical claims information to allow for improved care coordination and more precise risk-adjustment prior to enrollment through the CMS Consumer Directed Exchange program (CDX).
Population Management: Blue Button enables more timely updates to claims information so that the health care organizations are kept up to date of any changes to their patients and can reduce the manual burden of Claim and Claim Line Feed (CCLF) file retrieval for Accountable Care Organizations (ACOs) in the BCDA (Beneficiary Claims Data API Program).
Medication Adherence: Stand alone Prescription Drug Plans (PDPs) will receive Medicare Parts A and B data through another CMS program, AB2D. Through Blue Button, this enables them to calculate medication adherence as well as gain visibility into the care coordination needs of their patients, information that was previously unavailable to them.
Plan Matching: Participating plans can generate insights to empower the beneficiary to choose the plan most appropriate for them in their “shopping” experience. Using their full Blue Button claims history, beneficiaries can be reminded of all previous conditions, procedures, and medications in order to ensure the selection of a plan that matches their needs through the CMS CDX program.
Gaps in Care: Systems can generate patient lists and actionable insights at the point in care to equip providers with the necessary information to close those gaps and reduce clinical variation. Through another CMS program, Data at the Point of Care (DPC), providers are able to use the Blue Button claims information while treating a patient in order to best inform their care approach.
To better understand Blue Button, these programs, as well as how CareJourney can help, let’s dive a bit deeper into the specifics:
The Technical Specifics
Today’s Blue Button API allows for developers to register a beneficiary-facing application that allows beneficiaries to grant applications access to four years of their claims history. The Blue Button API uses the HL7 FHIR standard (v4) for beneficiary data and the OAuth 2.0 standard for beneficiary authorization.1
Over 1,300 fields from the CMS claims data warehouse are mapped into FHIR and surfaced across Patient, Coverage, and Explanation of Benefits FHIR Resources.1 The data model leverages a variety of industry-accepted coding standards such as BETOS, DRGs, NDC, ICD-9, ICD-10 as well as some standard FHIR and Medicare Billing systems. More information is available on the CMS GitHub repository. Beneficiary claims data is refreshed weekly and CMS recommends to fetch new claims data on a daily basis to ensure the most current information.
Blue Button Programs
As mentioned above, there are several key CMS programs that are grounded on the Blue Button movement.
Specifically, Blue Button leverages an API in the FHIR format (as described above) and is made up of different programs which align to a variety of use-cases. All of the programs deliver Bulk-FHIR claims data with the exception of CDX, which delivers claims data for one patient at a time. Click here for a list of vendors approved to accept Blue Button 2.0 data.
CMS Blue Button 2.0 or Consumer Directed Exchange (CDX)
This program provides FHIR-formatted data for one individual Medicare beneficiary at a time, to registered applications with beneficiary authorization.4 This program requires beneficiary or consumer consent so that the organization can acquire the beneficiary’s four years of claims data. A primary use case: data can be used by beneficiaries for plan shopping and for MA risk adjustment for new enrollees (if the registered application is owned by an MA plan). Beneficiaries must log into MyMedicare.gov and provide consent to access their data. The most difficult part of CDX is getting beneficiaries to consent to send information to the apps they trust. Two productionalized examples of CDX are leveraging the shopping experience and scheduling appointment workflows.
Shopping Experience: When a consumer logs into a plan website to choose the health plan most appropriate for them, they can select the “Estimate your drug costs” link which takes them to the MyMedicare.gov page to allow them to consent to share their Blue Button data. The plan then will use that information to calculate their drug costs to assist the consumer in choosing the right plan for them.
Scheduling an Appointment: When a consumer logs into an application or portal to schedule an appointment with a provider in network, they are given the option to consent to sharing Blue Button data to provide historical information to the provider to improve care coordination.
CMS Blue Button Beneficiary Claims Data API (BCDA)
This program provides clinicians with claims data for treatment purposes. This program allows for Shared Savings Program ACOs to use the FHIR-based API to retrieve bulk Medicare Claims data related to their assignable or prospectively assigned beneficiaries. This program is currently only available to ACOs and is not yet ready for use with Direct Contracting entities and other organization types. The BCDA program is intended to allow Shared Savings Program ACOs to4:
- Improve ease of access to bulk beneficiary claims data
- Decrease the time for CMS to implement any required requested updates to support the ACO program
- Reduce burden on ACOs for changes to the data or data format
- Enhance efficiency by enabling system-to-system communication and reducing the need for manual intervention to retrieve and manipulate the data
It should be noted that although the BCDA program does not require individual beneficiary authorization, beneficiaries can opt out of having their data shared with the ACO. It should also be noted that although CCLF files are not going away, the BCDA API can be substituted to allow for more timely, supplemental claims updates and for system-to-system communication and data transfer, reducing the manual burden of CCLF file retrieval.
CMS Blue Button Data At the Point of Care (DPC)
This program allows clinicians the ability to access their patients’ information within their clinical workflow, enabling the delivery of high-value care. This program requires that the data is shown to the provider at the point of care. Methods include display in the provider’s EHR or in an application of their choice. Many organizations are considering Substitutable Medical Applications, Reusable Technologies (SMART) on FHIR apps to achieve this outcome. SMART on FHIR enables your EHR to connect to apps seamlessly and most EHRs already support the specification, removing a potential barrier for program adoption.
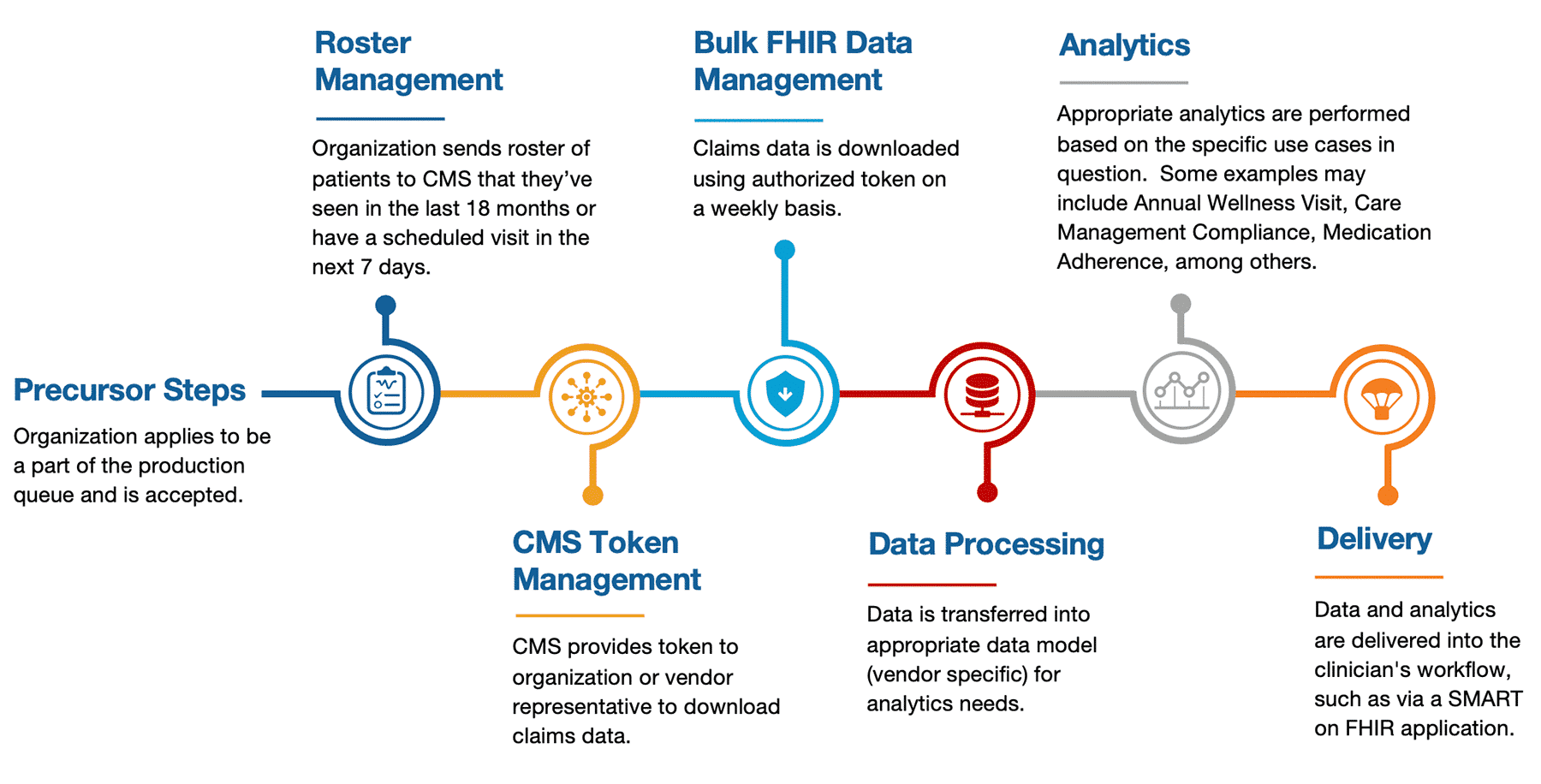
Under DPC, healthcare providers must assert to CMS they have a treatment relationship with a patient via an attribution roster. After verification, CMS will update the Bulk-FHIR claims data sent to the provider’s organization for the verified patients and their histories. While BCDA provides bulk data files to ACOs for their beneficiaries assigned to the ACO, DPC provides bulk data files to fee-for-service providers for their active patients, regardless of the ACO affiliation. As a part of the CMS patient verification process, they look for the patient having a visit (with the provider) within the last 18 months and with a scheduled visit in the next 7 days.
As of November 2020, provider organizations representing over 100,000 providers have requested access to the DPC pilot program and have access to the synthetic test data.2
CMS Blue Button Claims Data to Part D Sponsors (AB2D)
This program allows PDP sponsors the ability to request access to Medicare Parts A and B claims data for their enrollees. Using the claims data, PDP sponsors can promote the appropriate use of medications and improve health outcomes, among other benefits and the API provides key information to allow PDPs to track enrollee utilization, patient-provider treatment relationships, and patient history to aid PDPs in their goal of providing the best support to their enrollees.
Ultimately, AB2D enables PDPs to improve care coordination and optimize therapeutic outcomes through medication adherence. With the hopes of improving care coordination, AB2D will give them more insight (in near real-time) into the beneficiary’s history as well as providers treating them enabling PDPs to prevent adverse healthcare outcomes (i.e., preventable emergency department visits, hospital readmissions) by improving a beneficiary’s treatment plan. With this insight, PDPs have a better chance of promoting medication adherence, a financial incentive of the Star Ratings program.
CARIN Alliance Payer Blue Button / Common Payer Consumer Data Set (CPCDS)
Although this program is not explicitly part of the CMS Blue Button Program, this initiative is intended to assist government-regulated health plans in meeting their regulatory requirements to exchange data with consumers and other health plans by July 2021. CPCDS was developed by the Health Plan workgroup using a consensus-based approach, which has resulted in mappings of claims data to FHIR Resources that match the Blue Button 2.0 API profiles.
The Bigger Picture
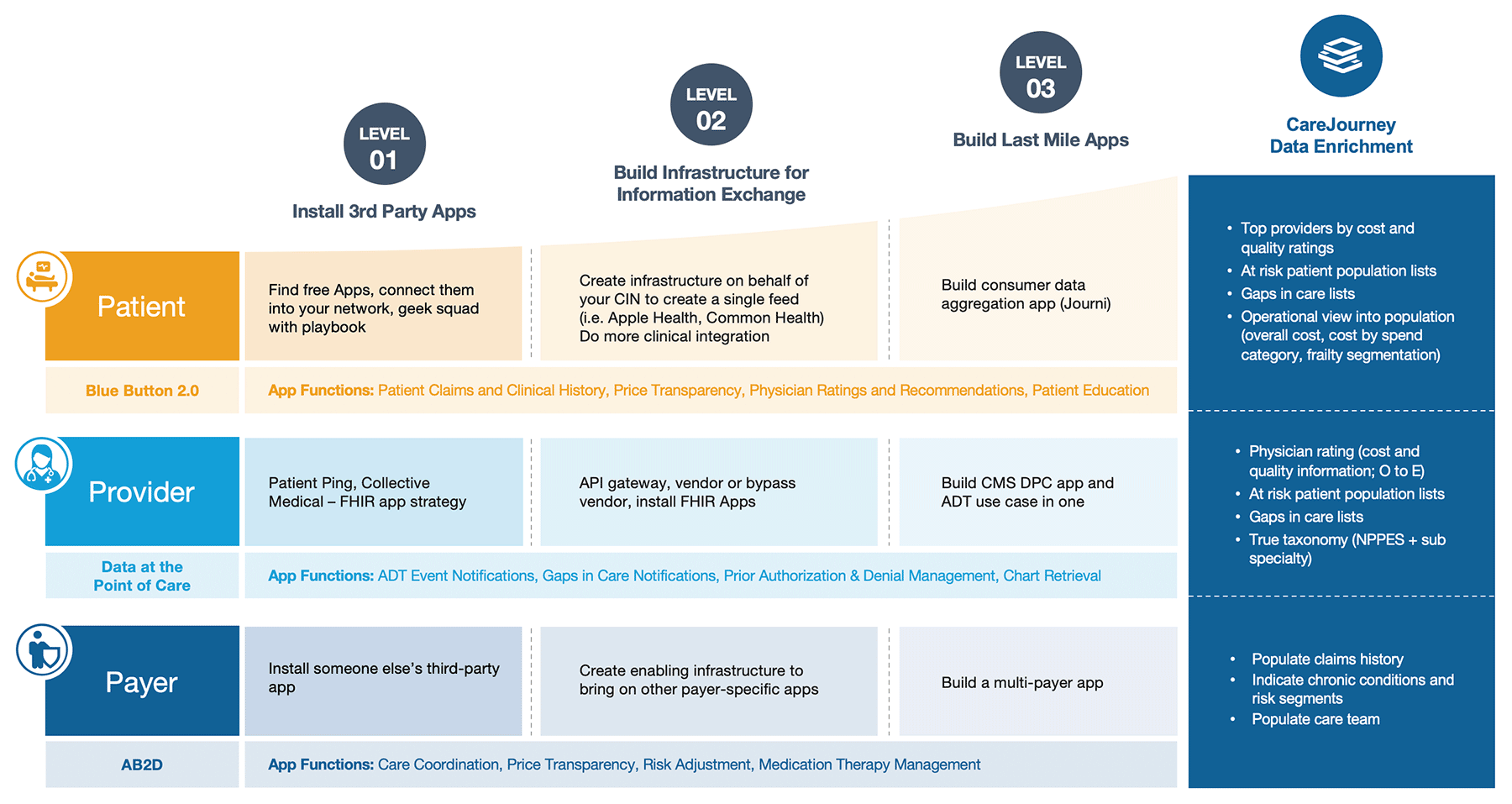
Health systems are pursuing “Blue Button” services in order to strengthen patient trust, improve care coordination, and build a new Health Information Exchange (HIE) pathway built upon consumer-directed exchange (outside of HIPAA).
Beneficiaries are highly interested in accessing their information electronically, using it to make health decisions and track progress toward their goals. Blue Button 2.0 has the potential to change the ways beneficiaries engage with health information, making it possible to aggregate and share health information with multiple health care providers via an application that helps them better organize, understand and act on their health data. Competition among application developers will increasingly focus on earning beneficiaries’ trust, akin to a “health information fiduciary.”
Health systems can better allocate care managers towards patients with higher priority coordination gaps. With Blue Button data, health systems can identify complex and chronic conditions by tapping into information generated outside of the network. Communication and trust are also improved when providers incorporate information generated between visits at the point of patient contact, including for the purposes of medication reconciliation or to enable transitional care management by identifying a patient’s Primary Care Providers.
Blue Button 2.0 integration can help create a centralized application for a patient’s digital healthcare data. As patients exercise their “right of access” to their medical records, a trusted centralized application will facilitate how data is accessed and exchanged, including enabling clinicians to “subscribe” to relevant patient updates via apps rather than dig for it within the EHR. This integration enables the technical infrastructure required for consumer-directed data exchange, while helping to address many of the non-technical barriers, including “information blocking”.
Finally, Blue Button 2.0 is enabling marketplace innovation – with application developers focused on reducing burdens on caregivers, personalizing “navigation decision support” for referrals, screening for low-value care, simplifying care team communication, and “one-click” scheduling, among others.
Blue Button Processing
While there are slight differences in the workflow for each of the Blue Button programs, below is an example workflow (DPC).
How CareJourney Can Help
Reach out to CareJourney for more information on how we can assist you in your Blue Button needs. Once up and running, CareJourney also offers data processing and analytics to members with Blue Button 2.0 data. For more information, please check out our work with BlueRock Care and Trusty.care as we all join hands to empower patients, caregivers, and providers with transparent information. For more information, reach out to your Member Services Rep or fill the form on this page.
- CMS Blue Button 2.0.Retrieved from https://bluebutton.cms.gov/
- CMS (November 2020). MyHealthEData Fact Sheet. Retrieved from https://www.cms.gov/About-CMS/Story-Page/MyHealthEData-fact-sheet.pdf
- CMS.gov. Blue Button® 2.0: Improving Medicare Beneficiary Access to Their Health Information. Retrieved from https://www.cms.gov/Research-Statistics-Data-and-Systems/CMS-Information-Technology/Blue-Button#:~:text=The%20Blue%20Button%20service%20was,via%20the%20MyMedicare.gov%20portal
- CMS. Beneficiary Claims Data API. Retrieved from https://bcda.cms.gov/
