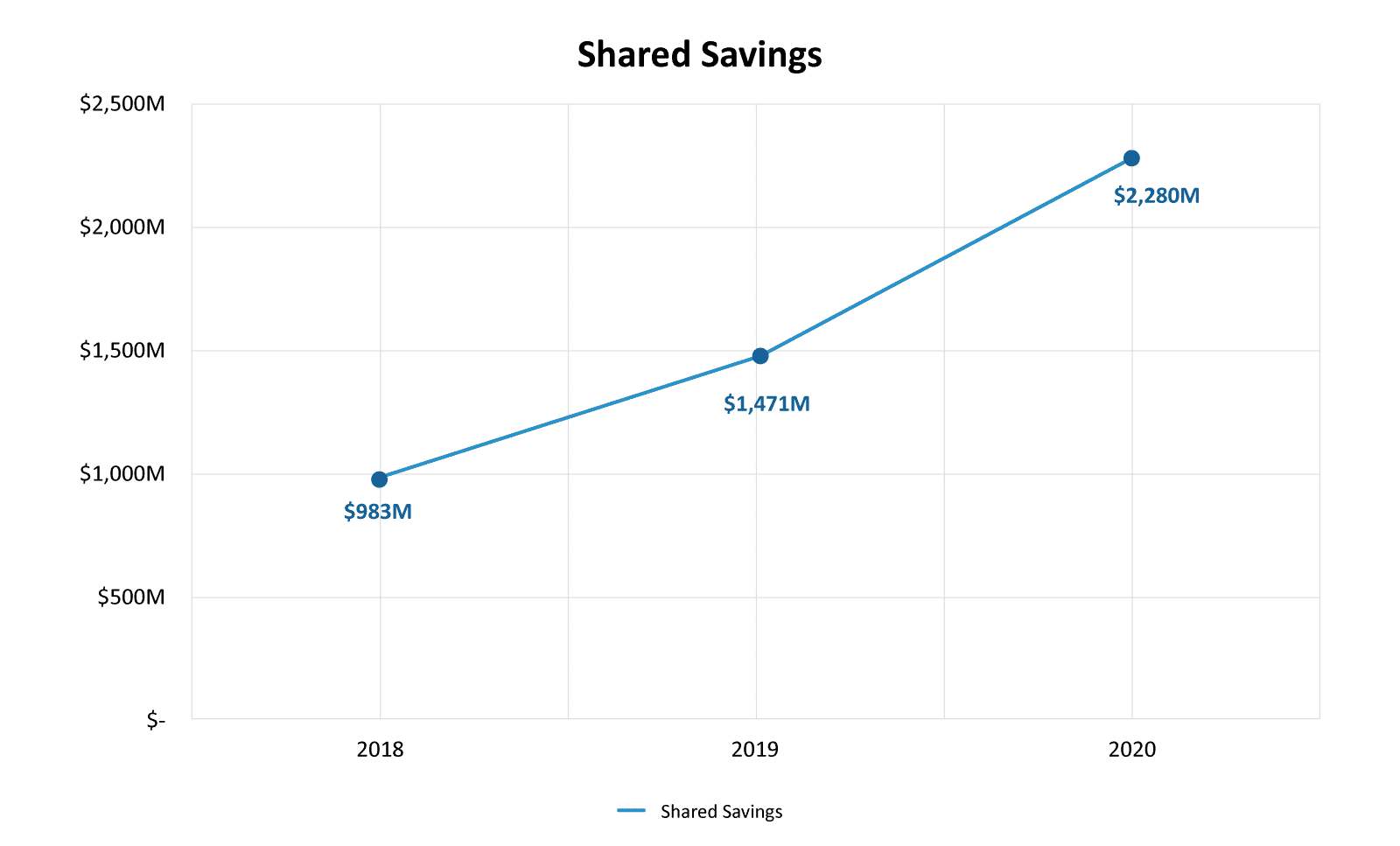
The Medicare Shared Savings Program (MSSP) is the largest value-based care program from the Center for Medicare & Medicaid Services (CMS) to date. As of 2020, there were 513 ACOs participating in the program, with a total shared savings of $2.28 billion.8 This program seeks to accomplish the following:
- Promote accountability among healthcare institutions for the care delivered to a patient population.
- Coordinate items and services to ensure that patients get the right care at the right time while avoiding unnecessary duplication of services and preventing medical errors.
- Encourage investment in high-quality healthcare and efficient healthcare services.
How do ACOs accomplish these goals, and how do they generate savings in the process?
In our previous blog, we profiled successful ACOs in the 2019 MSSP program and examined how they produced savings. In this blog, we will look at how those trends changed in 2020 and build upon those findings. Year over year we see a cohort of “All-Star” ACOs and 2020 is no different. In 2020, CMS saw the fourth consecutive year of net positive savings for the MSSP Program. Additionally, due to the COVID-19 Pandemic, CMS waived all shared losses for at-risk ACOs in 2020.
Shared Savings Program Fast Facts, ACO PUF Files9
2020 ACO Success At a Glance
Leveraging CareJourney’s 100% Medicare Fee-for-Service claims dataset, we analyzed available MSSP performance results from 2020. We analyzed utilization and quality metrics paired with total and per capita generated savings from 500+ ACO participants. Using this data we quantified the savings of each ACO based on their benchmark minus expenditure amount on a per capita basis.
| 2020 MSSP Performance Results: ACOs Quintiled by Total Savings per Beneficiary | |||
| ACOs Ranked by Total Savings per Capita | Avg Total Savings per Capita | Avg Number of Assigned Beneficiaries | ACO’s Per Quintile |
| Top 20% | $1,140.99 | 14,001 | 102 |
 |
$613.85 | 22,658 | 103 |
| $396.21 | 28,711 | 103 | |
| $189.05 | 22,272 | 103 | |
| Bottom 20% | $(280.97) | 15,632 | 102 |
In 2020, 83% of ACOs generated savings for Medicare FFS. By using total savings (benchmark minus expenditure) instead of using earned savings to calculate our ACO rankings, we were able to control for outside factors that impact an ACO’s “take-home” value; such as quality score, risk model, and savings rate. This also ensured consistent comparison in spite of the zero lower bound established this year by CMS. This allowed us to profile ACOs based solely on the performance of their savings in the program and understand top-performing ACOs through claims behavior.
At the highest level of analysis, we see two clear trends: top-performing ACOs have much higher savings per capita, nearly double than even the second performance quintile, and top-performing ACOs also have far fewer beneficiaries on average than the middle three quintiles. Looking back to 2019 we see that the average number of beneficiaries is mostly the same year over year, with the top quintile of ACOs averaging 14,001 beneficiaries in 2020, down slightly from 14,392 in 2019. Average total savings increased across quintiles in 2020, with the top-performing ACOs saving $1,140 in 2020, up almost 15% from 2019, where they saved an average of $934.
Profiling ACO Success: Which expenditure categories contribute to high or low spending?
Below is a table showing the expenditure category breakdown of PMPY spend among ACO’s in 2020.
| 2020 MSSP ACO Performance Results PMPY by Category | |||||||
| Quintile | Total PMPY | Part B PMPY | Inpatient PMPY | Outpatient PMPY | SNF PMPY | HHA PMPY | Hospice PMPY |
|---|---|---|---|---|---|---|---|
| 1 | 12,047.06 | 3,635.65 | 4,265.29 | 2,127.54 | 717.66 | 656.60 | 356.19 |
| 2 | 11,356.06 | 3,370.82 | 3,907.17 | 2,305.99 | 674.94 | 532.46 | 273.47 |
| 3 | 11,058.28 | 3,195.40 | 3,736.71 | 2,409.92 | 660.21 | 497.22 | 265.43 |
| 4 | 11,273.44 | 3,333.48 | 3,779.64 | 2,373.99 | 690.87 | 498.62 | 301.92 |
| 5 | 12,998.43 | 3,452.56 | 4,353.88 | 2,781.16 | 1,140.01 | 555.50 | 394.17 |
Across all quintiles, the highest expense category is Inpatient service on average, with the top-performing quintile of ACOs having 7% less spending per beneficiary than the bottom quintile. Similar to 2019, we also saw that among the top quintile of ACOs Part B services were much higher than among the other quintiles. Additionally, we see that the outpatient PMPY is the lowest among the top quintile ACOs.
ACOs in the top quintile also have significantly lower SNF spend on a per member per year basis than the bottom quintile, which reinforces the key strategy highlighted by CMS that encourages ACOs to focus on coordinating high-quality, low-cost care.2 Top quintile ACOs also had slightly higher spending on home health services than other quintiles of ACOs. Here we observe a substitutive effect wherein patients who are better cared for at home are steered toward accessing HHA services, which often offer better care at a better cost to patients. Not only is home health usually less expensive, but it is often just as effective as care in a hospital or SNF setting for many patients.³
Finally, one of the most interesting pieces of this data is that we see that total PMPY is actually higher among the top-performing ACOs than the next three quintiles. While this seems somewhat counterintuitive it is important to remember that CMS sets the benchmark based on a number of factors, including the risk of the population. This suggests that top quintile ACOs are likely treating a somewhat sicker population.
See National HCC Trends Across All ACOs.
Go to our free data dashboard to see hierarchical condition categories (HCCs) ranked by national prevalence.
How Does Your ACO Compare?
Purchase a custom workbook containing your ACO’s most and least prevalent HCCs, recapture rates, and more.
Profiling ACO Success: PCP Visits
Primary care physicians are at the core of ACO management; they help manage chronic diseases, foster patient health engagement, and coordinate proactive care services. Effective primary care management will then impact the spend and utilization of higher-cost services downstream.4
One place where we see the impact of the COVID-19 pandemic is in the reduction of PCP visits. While the trends identified in 2019 still continued in 2020, we saw an overall reduction of PCP visits across the board by 10-15%.
| 2020 MSSP Performance Results: PCP Per 1,000 by ACO Quintile | |||||||
| Quintile | PCP/1k 2020 | PCP/1k 2019 | |||||
|---|---|---|---|---|---|---|---|
| 1 | 9,832 | 12,454 | |||||
| 2 | 9,031 | 11,018 | |||||
| 3 | 8,710 | 10,812 | |||||
| 4 | 9,223 | 10,911 | |||||
| 5 | 9,772 | 11,777 | |||||
In 2019, we saw the top quintile of ACOs having 12,000 PCP visits per 1,000 beneficiaries which was also more than any other quintile. However, in 2020, we see a reduction in PCP visits per 1,000 across all quintiles, with the top quintile having only about 10k/1k. The bottom quintile actually obtained more PCP visits than any other quintile except the top with 9,772. One trend that we notice among top-performing ACOs is a higher utilization of primary care, but this data is also a reminder that what actually takes place during the PCP visits is important, as well. As we see in the next section, despite having almost as many PCP visits per 1k than the top quintile, the bottom quintile of ACOs still had lower compliance with preventive care and care management services.
Profiling ACO Success: Are Preventative Care & Care Management services being leveraged?
The next step of our analysis included how ACOs are performing on two different categories of care: Preventative Treatment such as Annual Wellness Visits & Flu Shots, and Care Management including Transitional Care Management & Advanced Care Planning visits. These services enable primary care practices to help patients stay healthy and out of the hospital by spending more time focused on prevention and wellness and, where appropriate, coordinating resources to ensure proper post-acute care management.5 Below, we see how these performances break out across quintiles.
| 2020 MSSP Performance Results: Care Models by ACO Quintile | ||||
| Quintile | AWV Compliance | Flu Shot | TCM | ACP |
|---|---|---|---|---|
| 1 | 44% | 57% | 24% | 12% |
| 2 | 39% | 58% | 21% | 8% |
| 3 | 42% | 57% | 22% | 7% |
| 4 | 41% | 58% | 23% | 7% |
| 5 | 36% | 54% | 19% | 6% |
The first and most important takeaway is that Annual Wellness Visit (AWV) compliance was 5% higher for the top quintile of ACOs than it was for the second quintile and 8% higher than it was for the bottom quintile of ACOs. AWVs are a special type of primary care visit where providers work with patients to perform a Health Risk Assessment (HRA) and create or update a patient’s Personalized Prevention Plan.1 Annual Wellness Visits are crucial to better clinical care. A study conducted by Aledade found that patients who received their first AWV experienced a meaningful reduction in adjusted total healthcare costs of 5.7 percent, with the greatest association seen for the highest-risk patients.5 Additionally, overall AWV compliance decreased for the first, second, and fifth quintile of ACOs from 2019 to 2020, but increased for the third and fourth.
Flu shot compliance, however, increased year over year with an average increase of approximately 3% across quintiles. While we can clearly see the impact of COVID in the reduction of AWVs and PCP visits, we see that it had little negative impact, or possibly even positive impact on the number of flu shots. As we prepare to evaluate 2021 performance of the MSSP program, adding the COVID vaccination rate will be another key metric that we will assess. Stay tuned for information in a follow-up post.
Other visit types include Transitional Care Management (TCM) and Advanced Care Planning (ACP). TCM is intended for primary care physicians to help facilitate the hand-off period following an inpatient, SNF, or other facility stay in a home or community setting. TCM visits can help prevent readmissions and reduce costs by ensuring a smooth transition of care.6 Through our data, we see that TCM compliance mostly held steady from 2019 to 2020 with the top quintile of ACOs maintaining their 24% compliance rate. All the while, the top quintile ACOs maintained higher rates of TCM compliance, with the bottom quintile having the lowest TCM performance.
ACP visits are used to establish the medical wishes of a patient if they become unable to make decisions.7 The trend in ACP services is clear, however, with the top quintile of ACOs having the highest ACP compliance, followed by a clear downward trend through the quintiles. As shown in the data above, ACOs with higher savings are more frequently leveraging ACP visits, and while it remains underutilized across the industry, we see a modest 1% uptick in usage with ACP compliance since 2019 in every quintile except the second quintile where it remained even.
One interesting trend: for the top quintile of ACOs, having more PCP visits is associated with higher rates of AWV, Flu Shot, TCM, and ACP compliance. But for the bottom quintile, more PCP visits is associated with a lower rate of AWV, Flu Shot, TCM, and ACP compliance. Visiting a PCP more often is usually beneficial, but it does not necessarily mean that the visits are accomplishing effective care management. It appears that not only is it necessary to have patients visit their PCP but also that those visits accomplish important care management activities. The top-performing ACOs are often making investments in provider performance management, using tools like CareJourney’s Provider Performance Index to provide feedback and coaching.
Profiling ACO Success: The Distressed Community Index
The Distressed Community Index is a five-part scale created by the Economic Innovation Group that examines economic well-being at the county level in order to illuminate the state of American prosperity. It incorporates seven components including high school graduation rates, vacant housing, prime-age employment, median income ratio, changes in employment and business, and the poverty rate. The DCI labels communities prosperous, comfortable, mid-tier, at-risk, and distressed.
CareJourney has overlaid our data on the Medicare FFS population with the Distressed Community Index to determine the relationship between Distressed Communities and ACO Performance. The results are striking. At a high level, we see top-performing ACOs with better cost performance in distressed communities than in prosperous communities, while also having the majority of the beneficiaries in prosperous and comfortable communities. The chart below compares ACO patient volumes and PMPY across ACO Performance Quintiles and DCI Indexes.
| DCI | ACO Quintile | Total Member Months | PMPY |
|---|---|---|---|
| Prosperous | 1 | 7,215,624 | $11,396.13 |
| 2 | 11,507,965 | $11,136.48 | |
| 3 | 14,120,084 | $10,953.05 | |
| 4 | 14,441,857 | $10,837.52 | |
| 5 | 6,779,095 | $12,400.80 | |
| Comfortable | 1 | 4,330,407 | $12,508.48 |
| 2 | 7,227,793 | $11,586.10 | |
| 3 | 6,855,917 | $11,183.88 | |
| 4 | 5,463,056 | $11,135.42 | |
| 5 | 4,739,778 | $12,914.03 | |
| Mid-Tier | 1 | 2,081,539 | $12,033.43 |
| 2 | 3,753,557 | $10,954.83 | |
| 3 | 5,535,548 | $11,218.76 | |
| 4 | 2,801,734 | $11,339.73 | |
| 5 | 3,186,654 | $12,190.18 | |
| At-Risk | 1 | 1,539,155 | $11,826.27 |
| 2 | 2,431,980 | $11,254.93 | |
| 3 | 4,768,629 | $11,402.21 | |
| 4 | 2,746,506 | $11,268.58 | |
| 5 | 2,278,547 | $12,923.49 | |
| Distressed | 1 | 877,041 | $10,967.91 |
| 2 | 1,212,778 | $10,835.49 | |
| 3 | 2,128,289 | $11,722.21 | |
| 4 | 1,470,238 | $11,864.76 | |
| 5 | 859,894 | $12,673.92 |
When we analyze the data, we find that while the ACOs are operating fairly evenly across distressed communities in terms of cost, with the greatest variance in PMPY differences between quintiles coming through their PMPY costs in distressed communities. In the below chart, we show the variance in PMPY for distressed communities.
Distressed Community
| DCI | ACO Quintile | PMPY | Top to Bottom Quintile Variance |
|---|---|---|---|
| Distressed | 1 | $10,967.91 | $1,706.01 (13%) |
| 2 | $10,835.49 | ||
| 3 | $11,722.21 | ||
| 4 | $11,864.76 | ||
| 5 | $12,673.92 |
Next, when we examine the variances in PMPY among the top- and bottom-performing ACOs we see that not only is there large variance in PMPY within the DCI there are also large differences across the DCI, with the largest variance coming within the most distressed communities.
The below chart shows the difference in Average Total PMPY between the top quintile of ACOs and the bottom quintile of ACOs for each community.
| DCI | Top to Bottom Quintile Variance |
|---|---|
| Prosperous | $1,004.67 |
| Comfortable | $405.55 |
| Mid-Tier | $156.76 |
| At-Risk | $1,097.23 |
| Distressed | $1,706.01 |
Taken together, this information tells us that ACOs are performing best on PMPY measures in Distressed communities, while deriving most of their volume from the least distressed communities.
Need national-level and ACO-level insights?
Access our JumpStart Dashboard.
Explore with CareJourney
This analysis gives us one lens to view ACO performance but,there is no perfect answer for success in MSSP. Experiencing success in MSSP requires a robust, well-coordinated series of initiatives across the entire patient journey, one which often transforms the patient experience. In practice, there are trends across ACOs that earn high-caliber savings. Many organizations that meet with success have a strong focus on controlling inpatient spending and providing better coordination and management of post-acute care.
CareJourney is actively engaged in exploring and investigating the drivers of ACO success as well as understanding the real world impacts of a successful value based approach to patient care, and is pursuing in depth research to understand the value to the patient of value based care, and what it truly means to be a top ACO.
In the meantime, there are several ways in which CareJourney can further support value-based organizations to drive actionable next steps from these insights, including:
- Evaluate the potential savings in switching the site of service for procedures, imaging, and labs for an attributed population.
- Track care management compliance from all levels of an organization: patient, provider and group levels.
- Understand utilization of services from an attributed population and cultivate strong preferred provider and facility networks.
- Understand provider performance and provide the insights needed for performance management conversations.
- Leverage CareJourney claims ingestion and transformation Population Insights tool to track care interventions in real time.
Many CareJourney members are top-performing ACOs, including Rush Health, PBACO, Privia, Silver State, Louisiana Physicians ACO, and South Texas ACO Clinical Partners. Collectively these members made over $200 million in shared savings. If you are currently a member and interested in how CareJourney can help you gain insights into designing and managing a value-based organization, please reach out to your Member Services representative for more information. If you are not a CareJourney member, please email us at jumpstart@carejourney.com, or you can learn more by requesting a meeting.
Not ready for a meeting? Check out our resources to learn how CareJourney helps payer, provider, and pharma organizations reduce the total cost of care and improve care quality.
- Medicare Wellness Visits. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/preventive-services/medicare-wellness-visits.html
- Medicare Program Shared Savings Accountable Care Organizations Have Shown Potential For Reducing Spending And Improving Quality. (2017, August). Department of Health and Human Services. https://oig.hhs.gov/oei/reports/oei-02-15-00450.pdf
- Medicare Home Health Beneficiaries. (2021, April 26). CareJourney. https://carejourney.com/medicare-home-health-beneficiaries/
- Paying More for Primary Care: Can It Help Bend the Medicare Cost Curve? (2012, March). Commonwealth Fund. https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_issue_brief_2012_mar_1585_reschovsky_paying_more_for_primary_care_finalv2.pdf
- New Study: In Physician-Led Accountable Care Organizations Medicare Annual Wellness Visits Are Assoc. (2020, December 11). Aedade. https://resources.aledade.com/press-releases/new-study-in-physician-led-accountable-care-organizations-medicare-annual-wellness-visits-are-associated-with-improved-health-care-quality
- Ballard, J. (2018). Effect of Ambulatory Transitional Care Management on 30-Day Readmission Rates. PubMed. https://pubmed.ncbi.nlm.nih.gov/29745236
- What is Advanced Care Planning? https://www.cdc.gov/aging/advancecareplanning/index.htm
- ACO PUF Files. https://data.cms.gov/medicare-shared-savings-program
This guide presents quick tips on implementing network selection, management, and optimization using the CareJourney Index Cost and Outcome Scores.
Watch this webinar featuring leaders from top-performing ACOs in Medicare Shared Savings Program (MSSP).
QIP is an Accountable Care Organization made up of physicians in private practice, working in coordination to care for over 7,000 lives in Kentucky and Southern Indiana.
