The US Opioid Crisis Continues to Grow
In our previous blog Opioid Epidemic, Part 1: The Prevalence of Opioid Use Disorder and Impact of Distressed Communities, we utilized Medicare Part D data (over 40 million enrolled beneficiaries) to highlight the growing prevalence rates across the board in the U.S. In short, the key findings were:
- Prevalence has doubled across the board
- OUD Prevalence Rates consistently on the rise, but significantly higher in some states
- Variation is stark even at the county level
- OUD increase fell year over year in 2017
So how are these patients obtaining such high volumes of opioids? Who is prescribing and where are patients filling these prescriptions? Read on to find out.
Note: An Opioid Use Disorder (OUD) Indicator represents an individual patient and is classified as any diagnosis, procedure, hospitalization, emergency department visit, or utilization of medication-assisted therapy (MAT) found in claims sourced from ICD, MS DRG, or HCPCS Codes.
The Pharmacy’s Role in the Opioid Epidemic
Pharmacists may often be overlooked when you think of a care team, but in reality they have a unique opportunity to impact opioid misuse. Not all will solve a murder or discover a clinic illegally prescribing opioids, like Dan Schneider did in Netflix’s The Pharmacist, but Pharmacists have the opportunity to provide education to both patients and providers. They can help guide patients to correct treatment for pain/dependence, while assisting physicians with patient monitoring.
Even though pharmacists have such a unique opportunity, they are seldom the focus of claims data analysis. It’s possible that this is because prescription data is harder to come by than professional services claims. CareJourney’s access to Medicare Part D claims through the CMS Innovators License allows us to analyze prescription claims through the lens of either the prescribing physician or the pharmacy where the prescription was filled.
Understanding Provider-Pharmacy Relationships
Utilizing Medicare Part A, B, and D claims and a patient-grouping algorithm, we have the ability to identify patient cohorts, such as an opioid use disorder (OUD) cohort, and attribute their care to providers that are considered responsible for that specific condition or set of conditions. Built into our Cohort Atlas offering, this attribution includes pinpointing the patient claims most relevant to the specified condition and connecting which providers are associated with those claims through diagnosis and procedure codes. For example, we can identify which opioid use disorder patients in a geography are attributed to providers, determine source cost, outcomes, and utilization metrics on that cohort of patients, and then compare metric performance across providers. This allows network builders to choose the appropriate doctors for specific patient populations, and it allows performance managers to identify opportunities for improvement tied directly to patient conditions and outcomes.
Our Custom Report Showing Impact on Total Cost of Care
Fill the form to download our report that explores individual pharmacy and aggregated state, and county claim rates and cost of opioid claims toward opioid use disorder (OUD) beneficiaries and/or non-opioid use disorder beneficiaries (OUD).
Including both specialists and primary care physicians, we can tie pharmacy, facility, Accountable Care Organization, and health system affiliations to attributed providers to understand how organizational structures impact the patient total cost of care. In further understanding the care patterns within Medicare, we can connect drug utilization rates with Part D data, and aggregate at the pharmacy level.
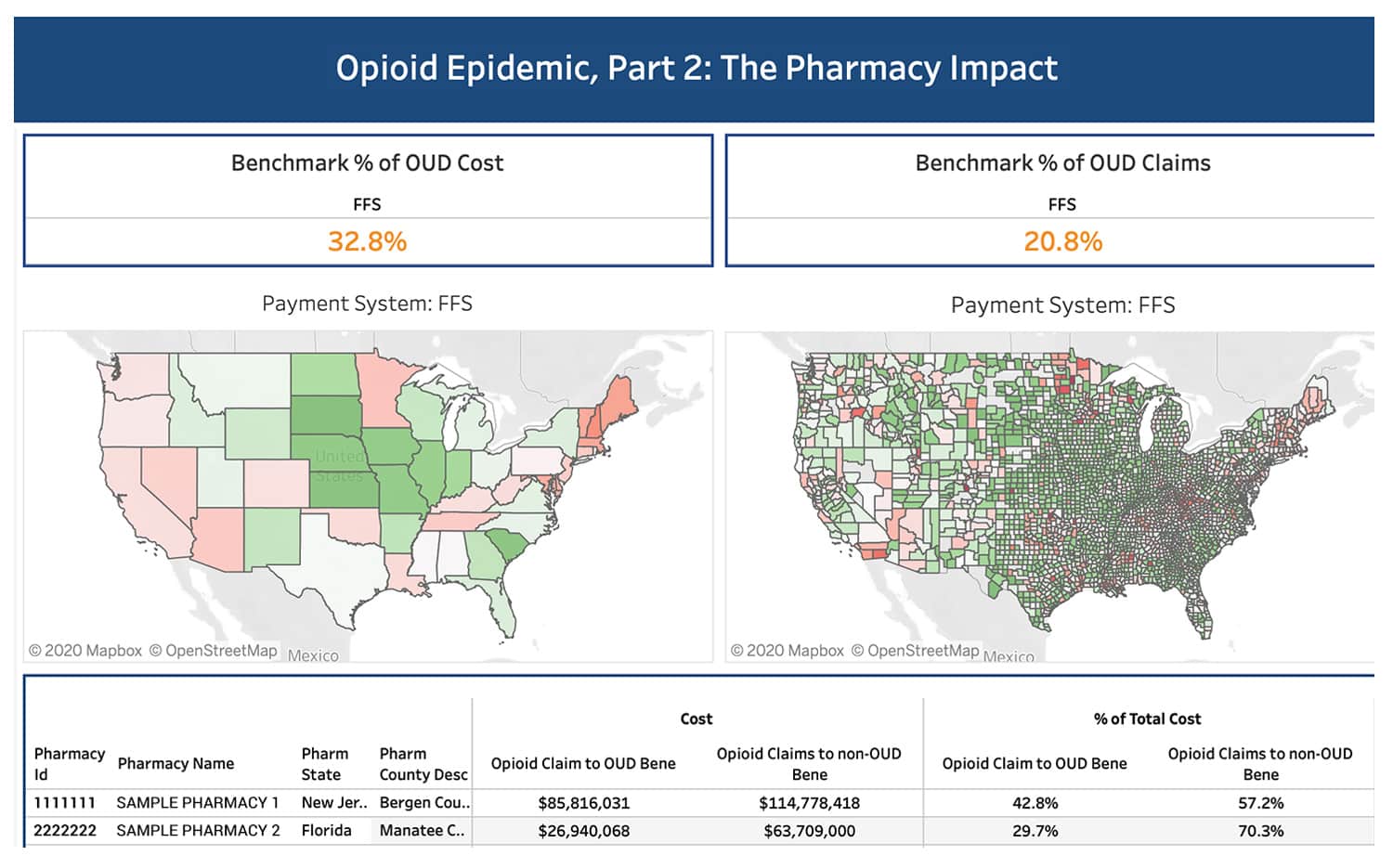
Data Definition: % of Opioid to OUD = Opioid prescription cost to beneficiaries that received an opioid use disorder indicator OVER all beneficiaries that received an opioid prescription in that calendar year.
Not a CareJourney Member?
Sign up for access to reports like this and more.
Key Findings
- National – Opioid use disorder (OUD) patients are prescribed a large portion of the total opioid prescriptions
OUD beneficiaries account for 20.8% of all opioid prescriptions filled nationally. - State – Highest rate of Opioid Prescriptions in Northeast US
In the Northeast section of the US there is a concentration of states with higher rates of Opioid prescriptions to beneficiaries with an opioid use disorder indicator (15+ percentage points above the national benchmark). - Pharmacy – Individual Pharmacy Insights
Within those select Northeast states there is a concentration of pharmacies with higher rates of Opioid prescriptions to beneficiaries with an opioid use disorder indicator.
Further Explore OUD Patients and Prescription Drug Data
There are a wide range of topics related to OUD patients that CareJourney is keen to explore. We aim to fully understand the additional costs and utilization that patients with OUD incur, as well as understand what treatments have been most effective. The CMS claims dataset allows us to explore these topics at extremely granular provider and cohort levels to identify actionable insights for our members. Further analyzing member claims down to the patient level, we can dive deeper into specific segments and highlight opportunities for care intervention or primary care coordination. For example, utilizing the High Need High Cost patient segmentation algorithm developed by the Harvard School of Public Health, we can explore overlaps of patients with opioid use disorder to create an opioid-intervention short-list to drive down cost and provide appropriate care for the patients that need it the most.
Analyses at the provider level can also inform the creation of OUD care teams for CMMI value-based care model participation in initiatives such as the Value in Opioid Use Disorder Treatment Demonstration Program. The purpose of this program is to increase access to care, improve health outcomes, and reduce long term Medicare expenditures for beneficiaries with opioid use disorder. Utilizing market participant analytics, we can identify doctors that provide medication assisted treatment (MAT) within a geography to include in an OUD care team.
In addition, there are endless research opportunities around Medicare Part D data. We recently posted an analysis of the tremendous savings opportunities around medication adherence. Furthermore, we can use the Part D data to infer chronic conditions of Medicare Advantage patients. This can give us a better understanding of what supplemental benefits plans may want to focus on based on their patient panel.
We would love to hear the ways that this data could be helpful to your organization! Please reach out to jumpstart@carejourney.com or learn more about our work by requesting a meeting below!
