How to Use Longitudinal Patient Data to Create a Better Continuum of Care
By Sam Crow and Ash Raghunathan
January 26, 2022
What is a Continuum of Care?
In an effort to provide better healthcare at lower costs, an increasing number of payers are focusing on providing a “continuum of care.” This model strives to identify and deliver the most appropriate care for an individual based on factors such as age, lifestyle decisions, genetic predispositions, prior care received, and more. The ultimate goal is to have a personalized relationship where providers guide a patient’s experience across their full care journey which may consist of preventative care, treatment or surgery, rehabilitation, and any follow-up health maintenance required.
While a continuum of care can be challenging to deliver, failure to do so results in significant payer costs: an estimated $200 billion annually for unnecessary medical tests, $150 billion for appointment no-shows and up to $2 trillion a year treating preventable long-term illnesses.
But healthcare decision makers have one tool in their tool box to help control these costs: longitudinal data. In this blog, we examine the complex challenges involved in gathering the longitudinal patient data required to provide an effective and efficient continuum of care.
What is Longitudinal Patient Data?
Longitudinal patient data tracks an individual’s health, risk factors, care usage (along with associated cost), and outcomes over time. This data, drawn from insurance claims, is typically used to provide a more individualized care experience for a patient while also tracking care effectiveness from the provider and payer viewpoints.
Because of its value in risk and cost forecasting, we consider deep, longitudinal data to be one of our six recommended healthcare data criteria.
What are the Longitudinal Data Challenges Involved in Providing a Continuum of Care?
One of the most significant challenges healthcare decision makers face when trying to deliver a continuum of care is that the way most care is delivered today makes gathering longitudinal patient data on adherence and care effectiveness difficult. In an ideal continuum of care, members of the care team would know everything about a patient: their demographics, medications, care episodes, adherence to treatment plans, genetic predispositions, age, lifestyle decisions and more. However, in most scenarios a patient must make their own appointments with a number of providers who rarely coordinate follow-ups, and no one provider possesses an overall view of any single patient’s care plan or overall health.
This decentralized delivery makes gathering patient data tremendously complex. Analysts looking to do so must sign data use agreements for every distinct provider in the continuum of care, and the process of accessing and formatting this data from large numbers of providers on a regular basis while maintaining HIPAA compliance on linking Personal Health Information to an individual is technically difficult (not to mention the significant amount of storage space required). As well, significant cleaning and standardization must be performed on provider data before it can be used for decision making.
All of these issues make cost prediction and risk adjustment for episodes of care extremely difficult. This is why longitudinal patient data that tracks care episodes and outcomes for healthcare providers over the multi-year time periods required for accurate forecasting is such a critical component to tracking patient progress through a continuum of care.
What Types of Longitudinal Patient Data Are Available?
A number of longitudinal claims datasets are available to healthcare decision makers, each of which carries its own benefits and drawbacks:
Medicare Data
The Center for Medicare Services (CMS) provides all claim data related to fee-for-service interactions with Medicare providers. CMS data has the benefit of being one of the largest healthcare data sources in the country (70M lives covered), and as such represents some of the best longitudinal patient data in the market. However, CMS data will have a very limited view into care episodes for anyone under 65.
Medicaid Data
Medicaid is state-run, with each state having different policies governing how it provides patient data to third parties. As a result, quality and the data itself tends to vary by state.
Most Medicaid patients participate in a managed care model, which can limit data to individual encounters and make longitudinal tracking more difficult. Additionally, Medicaid’s data is limited to each states’ covered populations. These populations generally include low-income individuals, families with children, pregnant women, the elderly and people with disabilities, but will vary by state and will fluctuate as changes to individuals’ life circumstances cause them to fall out of the data.
Commercial Payer Data
Employer- or insurer-provided patient data can often provide significant continuum of care detail thanks to payer incentives to provide more information. However, the data sets themselves are proprietary, generally smaller, and are not commonly shared in a fashion that supports tracking over time. In particular, commercial payer data breaks down longitudinally whenever a patient switches providers, which is most common when relocating and/or changing jobs.
How Can Longitudinal Patient Data Improve Continuums of Care?
Longitudinal patient data helps healthcare payers improve efforts in three areas:
1. Care Appropriateness
One of the most valuable applications of longitudinal data is in the measurement of appropriateness, which evaluates how likely a particular treatment is the most efficient form of care for a patient at that time in order to avoid waste.
At CareJourney, our healthcare analytics platform uses longitudinal appropriateness data to rank providers by cost and quality index scores. This scorecard can be used to build a roster of high-quality providers for your care network, or to encourage existing providers to focus on treatments that provide better outcomes over time.
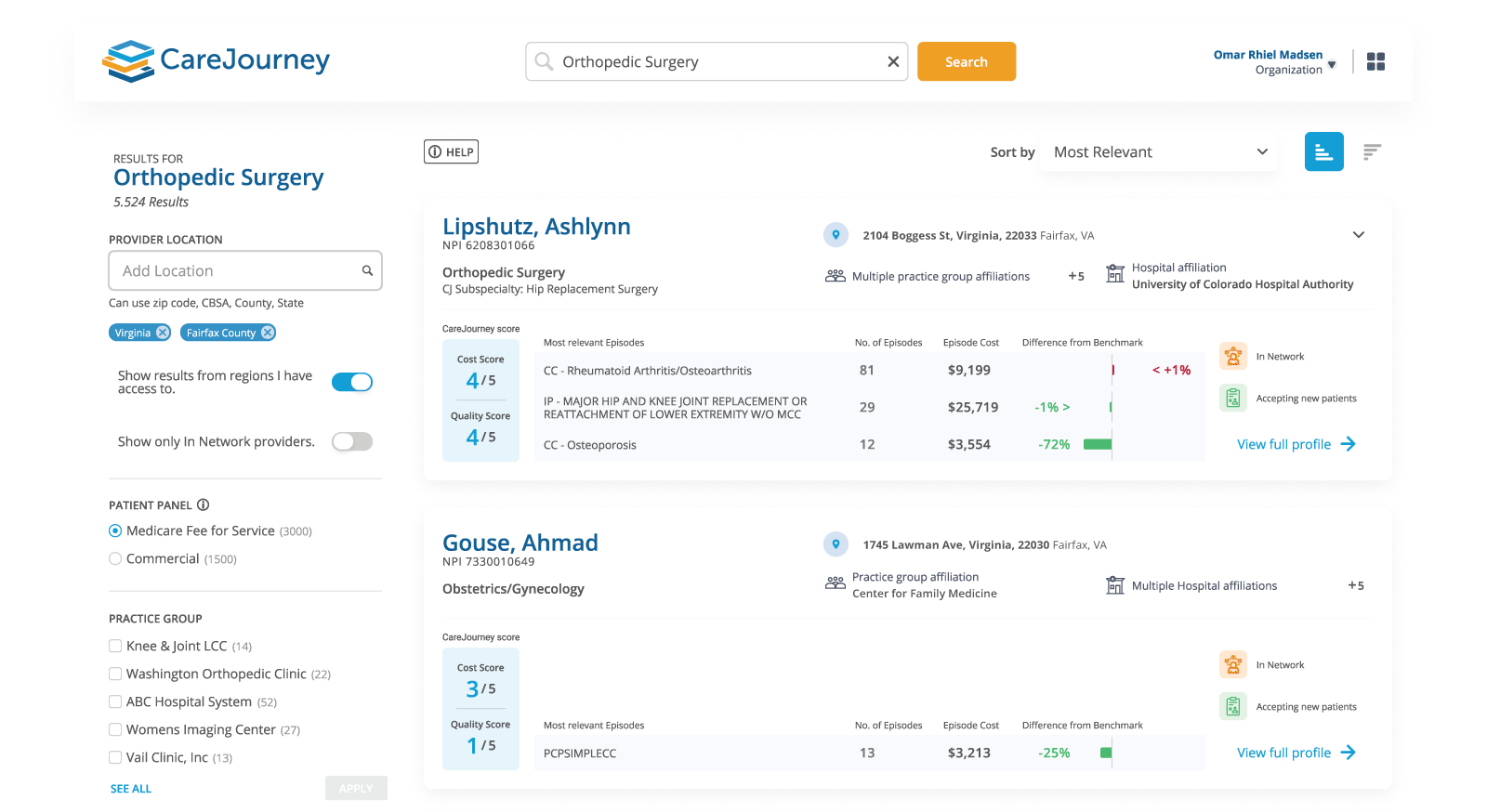
For payers looking to build a continuum of care, appropriateness measures can also help identify which procedures are most appropriate for a given patient cohort and help identify and resolve provider deviations away from the ideal flow of care. As an example, payers looking to improve care efficiency for older patients could review episode data for insights into the median number of care visits in a 70-year-old patient’s journey and then work to reduce that number.
2. Efficiency Improvements
Longitudinal data allows healthcare providers and payers to track quality and cost improvement measures over time in order to monitor the effectiveness of these efforts. For example, a payer that implemented a policy requiring drugs on a certain formulary tier be taken before more expensive medicines are authorized could review its patient data to see if this policy reduced costs and visits over time, or only added an additional step to its already fragmented continuum of care.
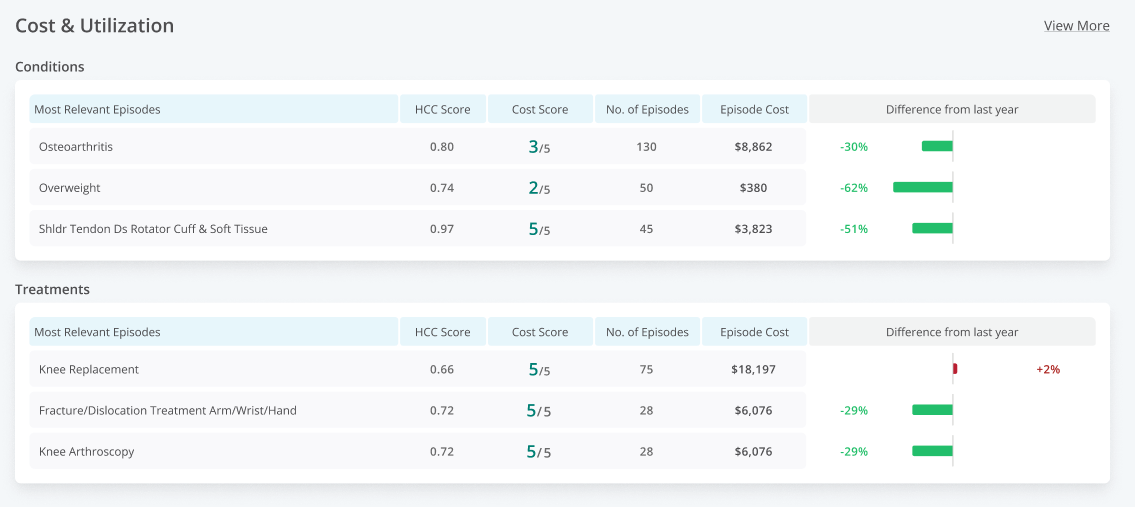
An episode grouper is particularly useful in this instance, as it aggregates granular claims data into a more clinically relevant bucket that provides visibility into the number of episodes for a particular health incident each provider reports in a given year. This data is ideal for identifying opportunities to improve care efficiency by episode condition.
3. Strategic Organizational Risk Management
Longitudinal patient data can also identify trends in community-level risk factors. For example, county-level data on COVID-related hospital stay durations could be used to uncover where COVID treatment practices are improving (you can review CareJourney’s data on how COVID-19 vaccination rates vary across different communities).
Another example would be monitoring the overall health of lower-income communities after efforts to improve access to care took effect. In this instance, longitudinal data could be used to determine the median cost for a Medicaid-eligible individual in order to support coverage decisions.
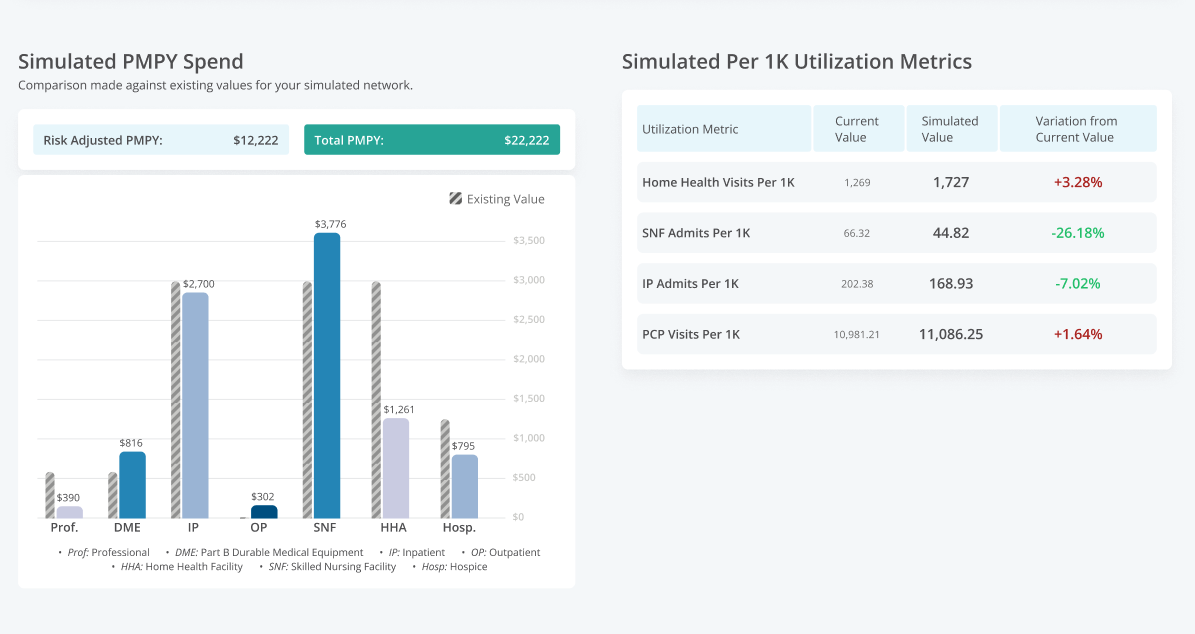
CareJourney’s platform allows healthcare payers to model utilization data based on real-world patient data in order to evaluate potential risk for a number of scenarios.
Explore with CareJourney
For more information on how CareJourney’s longitudinal data supports healthcare payer’s efforts to improve the efficiency of their continuum of care, please request a demo.
Not ready for a meeting? Check out our resources to learn how CareJourney helps payer, provider, and pharma organizations reduce the total cost of care and improve care quality.
