Background
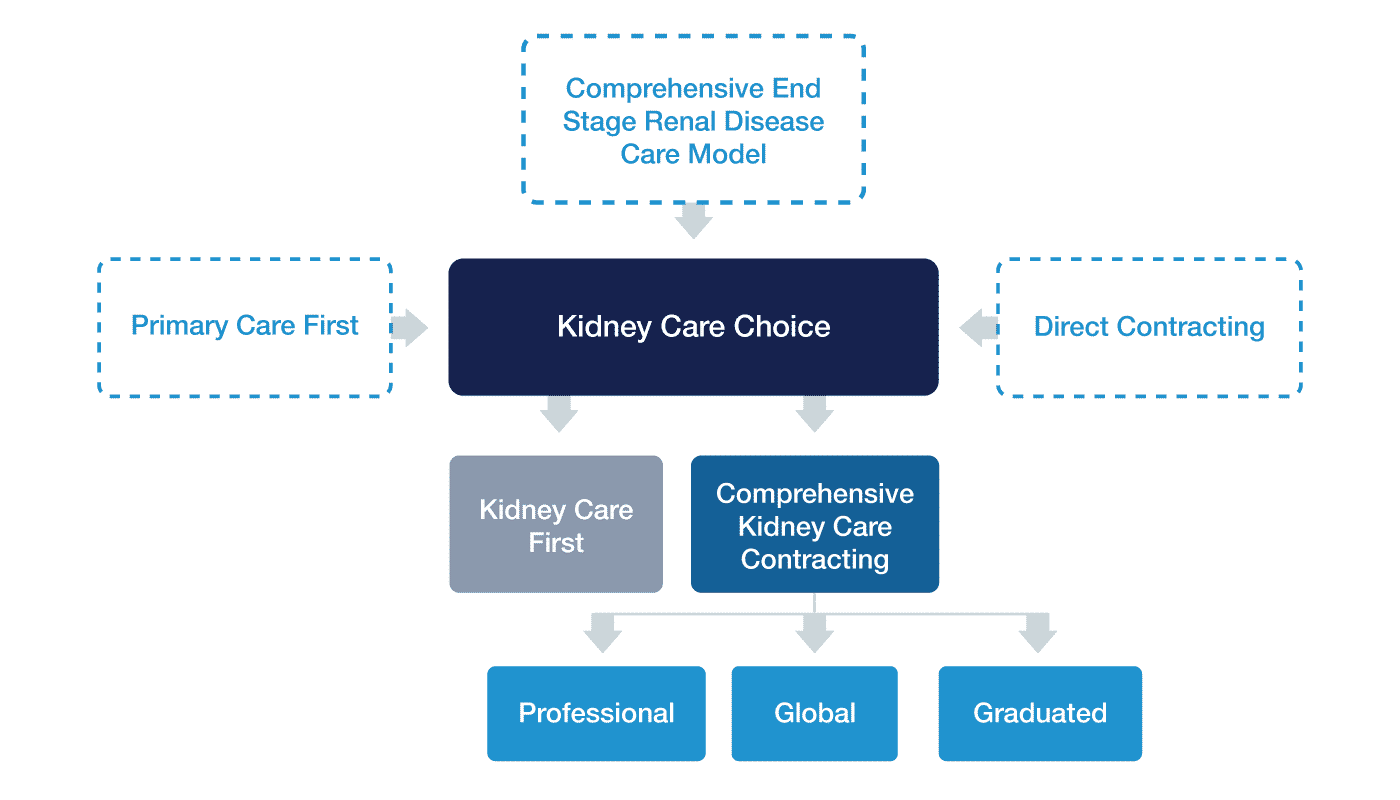
Kidney Care Choices (KCC) is a voluntary alternative payment model built on top of the Comprehensive End-Stage Renal Disease (ESRD) Care (CEC) model structure. The goal of the KCC model is to encourage nephrologists, dialysis facilities, and ESRD healthcare practices to focus on the total care of their patients, and incentivize kidney transplants for chronic kidney disease beneficiaries.
Beneficiaries are defined as attributed to a provider in the model if they are diagnosed with stage 4 or 5 chronic kidney disease (CKD) or ESRD, or if they were aligned to a participating KCC practice and then received a kidney transplant. According to CMS, more than 430,000 Medicare ESRD beneficiaries spend an average of 12 hours a week receiving dialysis at a center.1 The KCC Model is structured to incentivize participating practices to avoid putting patients on dialysis but instead perform a kidney transplant.
CareJourney is able to help organizations participating in the KCC model by providing an analysis of the various payment options. There are four payment options for the KCC Model: Kidney Care First (KCF), or a Framework for Improving Renal disease Support & Treatments, and Comprehensive Kidney Care Contracting (CKCC) which has three options; Graduated, Professional, and Global. These alternative payment models take concepts from the new Direct Contracting and Primary Care First models.
Our Analysis
Fill in the form on this page to view our analysis of Kidney Care Choices. Our analysis shows the average number of CKD beneficiaries per nephrology practice per state, the average number of ESRD beneficiaries per nephrology practice per state, and the average PMPM amount per provider per state.
Differences in the KCC Payment Models
The KCF payment option differs from the CKCC payment options in a few ways. Only nephrologists and nephrology practices can participate in the KCF model, while CKCC participants are required to include transplant providers and may include dialysis facilities. Additionally, while both KCF and CKCC receive adjusted payments for beneficiaries with CKD 4, 5, and ESRD, as well as the kidney transplant bonus payment, only KCF participants receive a performance-based adjustment through quality and utilization measures as compared to all KCF practices. This performance-based adjustment applies to the monthly and quarterly capitated payments.1
As of December 2016, more than 661,000 Americans have been diagnosed with kidney failure . However, only 193,000 are living with a functioning kidney transplant. In 2013, more than 47,000 Americans died from kidney disease, higher than breast or prostate cancer.2 Additionally, in 2018 nearly 750,000 Americans and an estimated 2 million people worldwide were affected by ESRD. By implementing the KCC model CMS is trying to have nephrologists and nephrology practices manage the overall health of their beneficiaries and promote nephrologists advocating for kidney transplants over dialysis regimens.
Succeed in ACO REACH
Check out our library of case studies, blogs, and webinars to help you succeed in Performance Year 2023 and beyond.
For participants in the KCF model, nephrologists and nephrology practices will receive adjusted fixed payments on a per-patient basis, with the payments adjusted based on quality health outcomes for the beneficiaries and utilization across the practice. For the top 10% of KCF practices, the performance adjustment is up to +30%. In comparison for the bottom 50% of KCF practices that are also in the bottom 25th percentile nationally, the performance adjustment is -20%. The -20% adjustment also applies to practices that fail to pass the Quality Gateway.
Quality Gateway measures are:
- gains in patient activation scores at 12 months
- depression remission at 12 months
- high blood pressure control
Utilization measures are:
- optimal ESRD starts
- hospitalization costs
- total per capita costs
Participating practices will also receive bonus payments for aligned patients who receive a kidney transplant, with bonuses paid out annually over three years while the transplant is successful and the patient is not on dialysis. Performance-based adjustments impact the monthly and quarterly prospective payments.
Based on the KCF payment model, participating entities are prospectively paid for their CKD and ESRD beneficiary populations. For beneficiaries with ESRD, payments will be made monthly at the 2-3 visit in-center rate for each aligned patient. For beneficiaries with CKD, payments will be made on a quarterly basis for a bundle of CPT codes listed below, at ⅓ of the 2-3 visit in-center rate.3 Since both of these rates are subject to the performance adjustment, knowing the number of beneficiaries and how participating entity rates in performance will allow a practice to plan their prospective monthly and quarterly payments accurately.
Our analysis calls out the average number of beneficiaries per organization in each state. For those who are enrolled in a KCC model, CareJourney can provide analysis around county-level and provider-level attribution, as well as Medicare Part A & B costs based on the attribution.
Comparison of KCC Model Options
| Payment Options | Similarities | Differences |
|---|---|---|
| Kidney Care First (KCF) Option | Beneficiary Attribution Logic:patients with CKD stage 4/5 or ESRD, and those who were so aligned before receiving a kidney transplant
Organization: includes nephrologists and nephrology practices Payments: Adjusted Monthly Capitated Payment (AMCP), CKD Quarterly Capitated Payment (CKD QCP), and the Kidney Transplant Bonus (KTB) |
Payment: also includes a Performance Based Adjustment (PBA) component that influences the AMCP and CKD QCP payment amounts |
| CKCC Graduated Option | Organization: must also include a transplant facility, and can include a dialysis facility
Payment: incorporates a shared savings/shared losses component at lower-reward, lower-risk |
|
| CKCC Professional Option | Organization: must also include a transplant facility, and can include a dialysis facility
Payment: incorporates a 50% shared savings/shared losses component |
|
| CKCC Global Option | Organization: must also include a transplant facility, and can include a dialysis facility
Payment: incorporates a 100% shared savings/shared losses component |
See Deeper KCC Analysis
Access the average number of CKD beneficiaries, ESRD beneficiaries, and PMPM amount per provider per state.
Methodology
Our methodology defines attributed beneficiaries based on the Request for Applications (RFA) published by CMS. The KCC Models specifically calls out beneficiaries with CKD stage 4 or 5, or ESRD. Please reach out to CareJourney for a more in-depth explanation of our methodology.
The attributed beneficiaries were determined by those with claims on nephrology related diagnosis codes, to align to one of two categories; CKD stage 4 or 5, and ESRD. For beneficiaries aligned to CKD stage 4 or 5, we looked at average paid Evaluation & Management (E&M) codes for CKD. Patients need to be aligned to a practice participating in the KCF model before receiving a kidney transplant. Therefore, no transplant patients were included in this report. For CKD beneficiary alignment, we are using the list of E&M codes listed in the RFA in Table 3.4 These codes are summarized in the table below.
| CKD QCP Included Services | CPT/HCPCS Codes |
|---|---|
| Office/Outpatient Visit E/M | 99201-99205, 99211-99215 |
| Prolonged E/M | 99354-99355 |
| Transitional Care Management (TCM) Services | 99495-99496 |
| Advance Care Planning (ACP) | 99497-99498 |
| Welcome to Medicare and Annual Wellness Visits | G0402, G0438, G0439 |
| Chronic Care Management (CCM) Services | 99490 |
Explore With CareJourney
Patients with CKD and ESRD are at higher risk of complications from COVID-19, as well as potential contact during dialysis treatments. If you are interested in evaluating the KCF or CKCC models or are interested in diving into your ESRD population from an MA perspective, please contact CareJourney for more information. CareJourney has two COVID-19 Blog Posts here: Responding to a (Digital) “Call to Action” on COVID-19 and Impact of COVID-19 on Accountable Care Organizations Short-Term and Long-Term.
- “Kidney Care Choices (KCC) Model.” Share, 2020, innovation.cms.gov/initiatives/kidney-care-choices-kcc-model/.
- “Kidney Disease Statistics for the United States.” National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services, 1 Dec. 2016, www.niddk.nih.gov/health-information/health-statistics/kidney-disease.
- Ketchersid, Terry. “KIDNEY CARE CHOICES: TRICK OR TREAT?” Acumen Physician Solutions, 28 Oct. 2019, acumenmd.com/blog/kidney-care-choices-trick-or-treat/.
- “Centers for Medicare & Medicaid Services (CMS) Center for Medicare and Medicaid Innovation (CMMI) Kidney Care Choices (KCC) Model – Request for Applications (RFA).” Centers for Medicare & Medicaid Services, 2019.
