Why is referral management important?
Care transitions that involve moving from one health care provider to another can often be stressful and daunting for patients; looking for high quality follow-up care while trying to manage costs can be complex. This process is equally cumbersome for nurses and care coordinators who want to ensure that they send their patients to the best in-network providers. Furthermore, the lack of a central and transparent process lends to the difficulty.
This makes referral management tools backed by evidence, experience, and a data-driven approach critical – which can allow the selection of the most appropriate provider, making transitions easier and helping improve the quality of care for patients.
What does a good referral look like?
At its very core, a good referral is one that allows a patient to continue their care journey with providers who can provide high quality of care while staying in-network so that costs do not escalate. Referrals based on objective facts instead of word of mouth or personal recommendations about a provider’s performance can lead to better health outcomes. To achieve this, nurses and care coordinators in charge of finding providers need better visibility into care transitions so that they can guide their patients for their next treatment. Specifically, they need the following:
- Key performance metrics: Performance metrics that help determine the overall quality and cost of a provider can give a quick insight into their performance, whereas more detailed metrics into treatments relevant to the patient’s needs and procedures performed can provide more specific insights.
- Benchmarks: Benchmarks are important metrics that help contextualize and compare the performance of the provider against standards in the area. They help answer the question: How does this provider perform compared to a standard in a particular geographic area?
- Geographic information: Travelling long distances can deter patients from keeping their appointments. Knowing which locations a provider operates from can be important for care teams to ensure that their patients do not have to travel far to seek follow up care.
- Network Status: Knowing whether a provider is in-network can be critical in helping patients prevent higher costs of care.
In addition to these important features, nurses and care coordinators also need information that they can quickly get access to at the point of care, and that is easy to understand, reliable and most relevant for the specific patient. This will enable them to make faster and better referral decisions.
What are the challenges in making good referrals?
Through CareJourney’s extensive support to leading provider groups and health systems, we have unearthed the challenges faced by nurses and care coordinators in making referrals. To start with, they have to rely on their memory or anecdotal evidence to find and recommend the right provider. Spreadsheets containing this information can get outdated quickly and it isn’t easy to systematically capture information based on word of mouth. Even when they have determined a potential fit, they still have to call the provider’s office to seek the most updated information such as: are they in-network or accepting new patients? Which locations do they practice from? What treatments and procedures do they perform? Commonly, the best-fit providers are located too far from the patient or are not in-network, making it more likely that the patient will discontinue treatment.
Gathering all this information before each patient referral can be cumbersome and time consuming, disrupting daily work flows.
Get an example of the data needed to make appropriate referral decisions.
View the volume of hand fractures in three different regions, and an example of the physician data that strengthens referral decisions.
How does CareJourney help improve referral management?
Our robust library of provider profiles within the CareJourney analytics platform helps health systems improve the quality of provider referrals and reduce out-of-network leakage. Easily search through the profiles, which are built on industry-leading, clinically-relevant analytics and insights on provider performance. In a single user interface, your care teams can simplify referrals directly at the point of care.
Quick Search
- Nurse and care coordinators easily search for providers using keywords such as specialty and subspecialty (powered by our sophisticated taxonomy algorithms) to quickly find the most relevant profile. They can get as granular as a specific treatment or condition based on the patient’s requirements, or a particular provider name or even NPI that they are interested in reviewing. Moreover, location based searching allows them to ensure that they are finding providers that are close to their patients.
- Narrow down your search by using a number of intuitive filters, including specialties, episodes, scores, and even by network status to see only those providers who best fit the patient’s requirements.
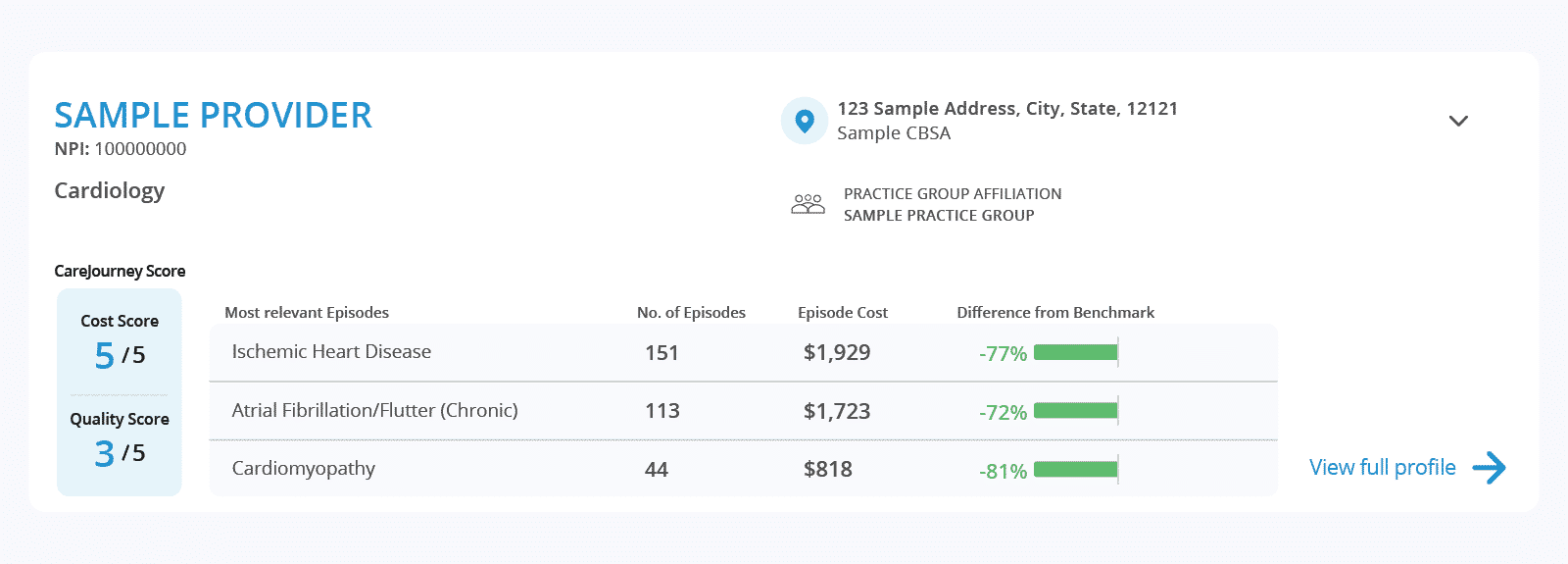
CareJourney’s Provider Performance Index (PPI)
- PPI is built on a comprehensive methodology that assigns a provider an overall cost performance and quality score. These scores help nurses and care coordinators quickly compare across providers on their cost efficiency and outcomes of care.
Longitudinal data
CareJourney provides powerful and insightful analytics which are based on our access to one of the most comprehensive claims databases in the nation, with activity across 200M+ Medicare FFS, MA, Commercial, and Medicaid lives. Much of the data is longitudinal, meaning we can analyze 100% of the claims activity for the patients that are attributed to primary care providers or undergo certain episodes of care with specialists.
- Use episode-level data to answer high-priority questions like: How many episodes has the provider treated that are related to the patients requirements? What is their cost of treating this episode? How much does it differ from a geographic benchmark?
- Surface other comprehensive performance information about providers, including their performance on quality measures, as well as cost and volume of the top procedures performed.
- Nurses and care coordinators also benefit from other important information about a provider like: is the provider in network? What locations do they practice from? And with which practice groups and hospitals are they affiliated?
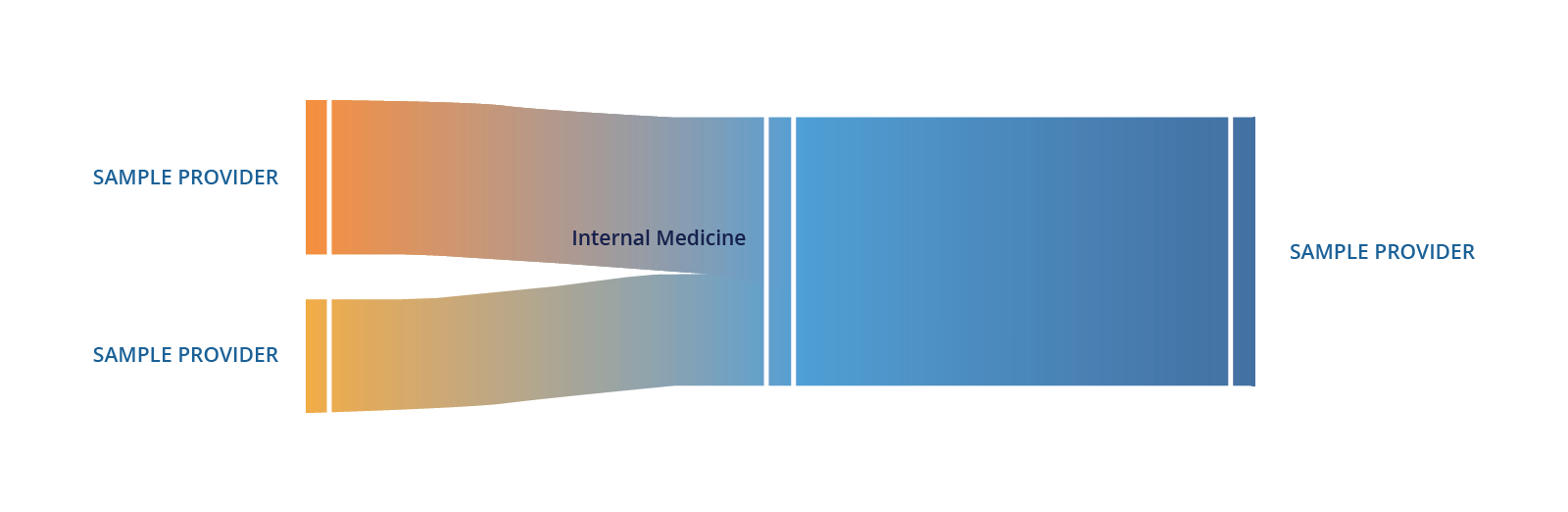
Referral patterns
Understanding a provider’s referral patterns is important to assess: (1) the quality of providers who refer to each other, and (2) if these providers are in-network. While the first enables nurses and care coordinators to determine if their patients will continue getting high quality care down the line, the latter helps understand referrals that are made in or out-of-network, to avoid unnecessary leakage. The CareJourney platform makes it easy for nurses to intuitively make the right decision at the point of care.
Nurses and care coordinators can easily adopt these analytics into their daily workflows to make better informed and more powerful referrals so that care transitions can become less complex and higher quality—both for them and their patients.
Existing members: request a demo today with one of our Member Services representatives and see how this tool can improve referral management at your organization. Not a CareJourney Member? Please contact jumpstart@carejourney.com and we will connect you with a representative that can share more information about our capabilities.
Explore with CareJourney
As you begin or continue the process of building and refining your network, request a meeting with our experts to:
- Identify prospective practice groups and providers to bring into your network,
- Evaluate your current provider network,
- Simulate network performance with prospective practice groups and providers.
Not ready for a meeting? Check out our resources to learn how CareJourney helps payer, provider, and pharma organizations reduce the total cost of care and improve care quality.
