This blog is part one of a series about ACO REACH. Read our second installment, Why Understanding Risk Scoring in the ACO REACH Model is Critical For Success.
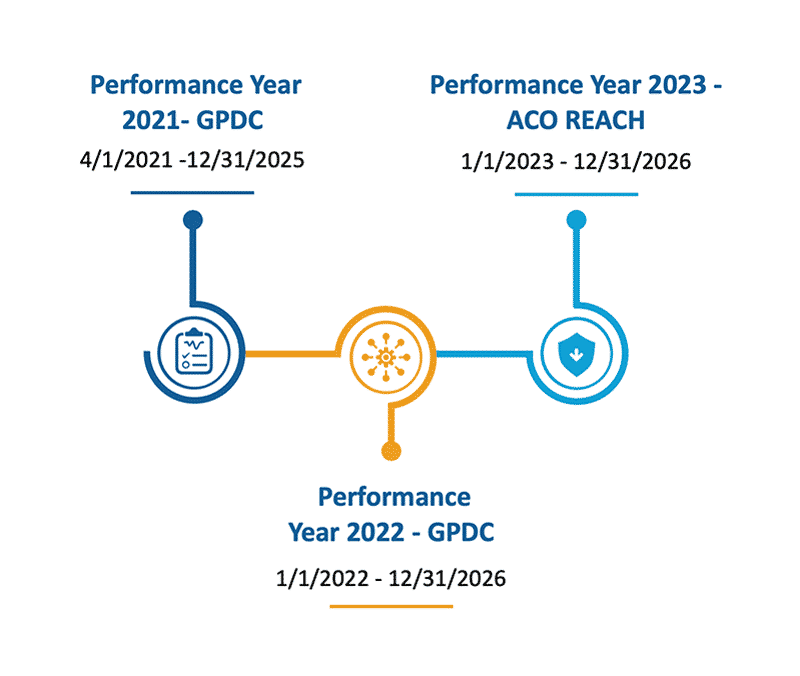
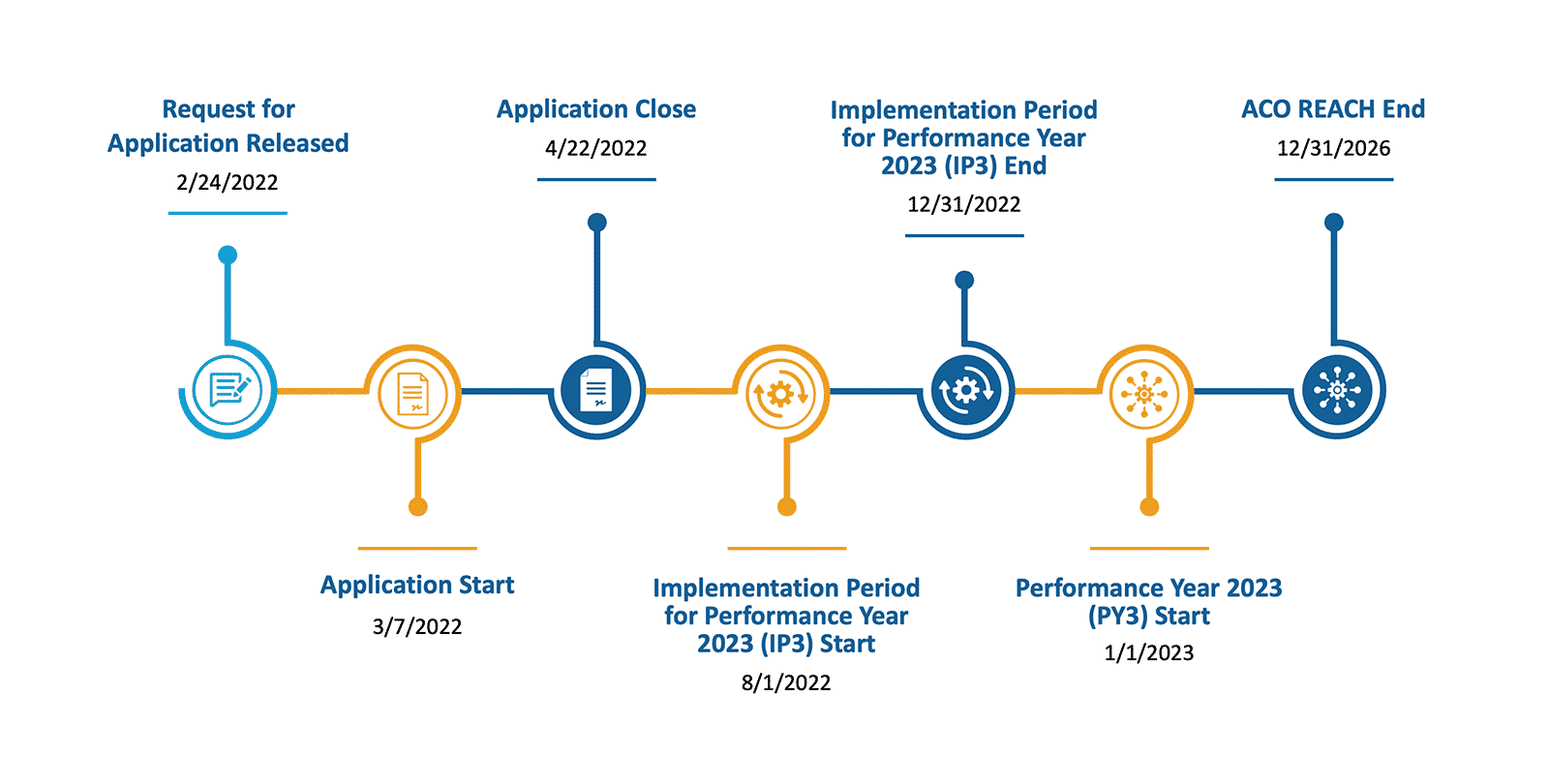
On February 24, 2022, the CMS Innovation Center released the details on a new payment model, ACO REACH. ACO REACH represents a series of changes made to Global and Professional Direct Contracting (“Direct Contracting”, GPDC) to respond to criticisms faced by the program. ACO REACH adds in exciting new components aimed at closing health equity gaps in keeping with the Innovation Center’s Ten Year Plan released late in 2021.
While ACO REACH and Direct Contracting share most of the same model components, there are some important differences. At a high level, ACO REACH addressed concerns about having funded entities in control of seniors’ healthcare by requiring 75% of the ACO’s governing body be controlled by participating providers – an increase from Direct Contracting’s 25% requirement. Additionally, ACO REACH makes it easier for smaller, less-funded groups to enter the model by decreasing the discount on the benchmark from a max of 5% to a max of 3.5% by the end of the model performance.
See Your County’s Equity Benchmark Score
This dashboard provides insights into the dual populations and the Area Deprivation Index of counties across the United States.
ACO REACH also responded to concerns of patient risk coding abuse by continuing with a cap on risk score growth of 3% being year over year to a 3% cap from a static base year, meaning that if the underlying demographics of the ACO do not change, risk scores can never grow more than 3% during the model performance period. ACO REACH seeks to bring more underserved beneficiaries into the model, beneficiaries who may be under-coded due to lack of utilization and beneficiaries who may be sicker. Recognizing these beneficiaries could cause an ACO’s risk score to grow more than 3%, the ACO REACH model provides for additional risk score growth if the underlying demographics (sex, age, disability, dual eligibility status) of the ACO shift from the base year. Read our deeper analysis on why understanding risk scoring is critical to success in this model.
One of the most exciting new components of the ACO REACH model is the focus on social determinants of health and health inequities. The model has multiple components geared towards identifying beneficiaries in need of extra assistance or who aren’t getting the correct care and closing those care gaps. The ACO REACH model addresses this in a few ways:
-
-
- Health Equity Plans: Each ACO will be required to develop and submit to the Innovation Center a Health Equity Plan. They will also be required to report their progress on the plan and outcomes from the plan. We will learn more about these requirements in future documentation.
- Benchmark Adjustments: ACOs who serve beneficiaries in the neediest decile (as determined by the beneficiary’s Area Deprivation Index plus dual eligible status) will receive a $30 per beneficiary per month (PBPM) upward adjustment to their benchmark for those beneficiaries. ACOs who serve beneficiaries in the bottom five deciles will have a $6 PBPM downward adjustment for those beneficiaries.
- Beneficiary Engagement Incentives and Beneficiary Enhancements: ACOs have the opportunity to provide beneficiaries with engagement incentives and in-kind benefits to encourage better management of chronic conditions. For example, an ACO could provide a hypertensive patient with a blood pressure cuff to use at home, or with a travel voucher to get to an appointment. Additionally, ACOs have an array of beneficiary enhancements they can choose from including a newly-added option allowing nurse practitioners to certify beneficiaries for certain needs such as hospice, diabetic shoes, cardiac therapy, etc., lessening dependence on physicians for these certifications.
- Required Demographic Data Collection: The ACO REACH model adds a requirement that ACOs must capture and report beneficiary reported demographic data to include race, ethnicity, language, gender identity and sexual orientation, which is the gold standard for demographic data. ACOs will be provided with a FHIR app to collect this data, or they can use an approved Excel template. While not required, ACOs are strongly encouraged to also collect SDOH data from beneficiaries. Gathering this data is a critical first step in closing care gaps for the underserved population.
- Adding Health Equity Experience to the Application: Finally, the Innovation Center has added a section to the ACO REACH application for potential ACOs to talk about their previous experiences in serving underserved populations.
-
Participating in the ACO REACH Model?
Learn how to be successful in the model.
Part of the Medicare Shared Savings Program (MSSP)?
Learn how to improve performance in MSSP.
The ACO REACH program also introduces data interoperability requirements and opportunities. Any agreement between an ACO and either a participating or preferred provider that involves the transfer of health records must comply with Federal interoperability standards. Additionally, with the required demographic data collection and the suggested collection of SDOH data, ACOs have the option of using a CMS provided FHIR app. This introduction of FHIR apps could be the catalyst needed for their development and widespread use. The use of FHIR apps can improve methods and the speed in which health data is exchanged while also radically lowering the costs imposed on providers who must currently use pricey third-party applications to report quality metrics and otherwise exchange health data.
ACO REACH: What Stays The Same?
-
-
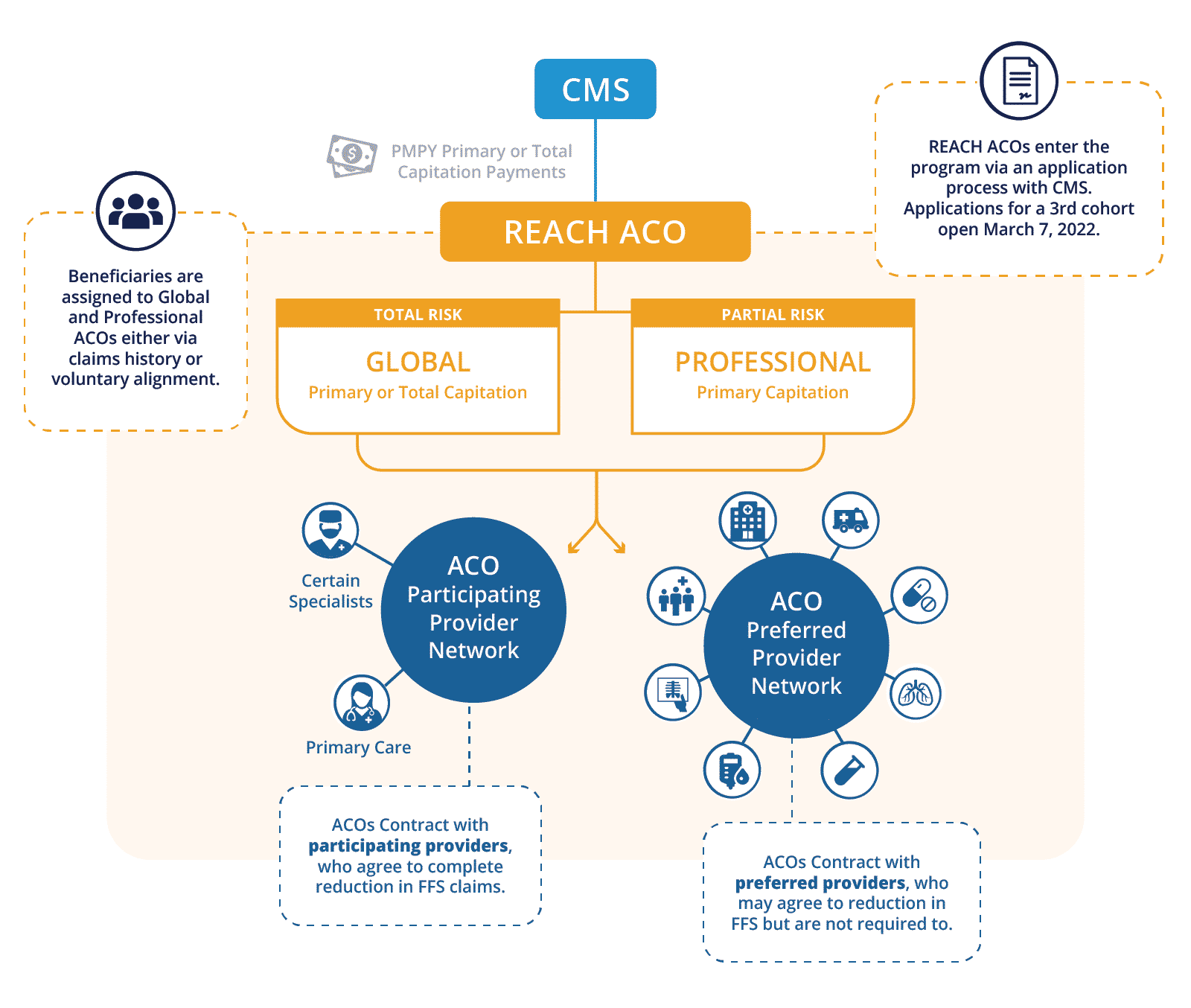
- ACO REACH will continue to have two tracks: Global and Professional. The Professional Track will remain as a primary care capitation only model with 50% shared savings and losses. The Global Track gives ACOs the option of primary care capitation or total cost of care capitation with ACOs taking on 100% of the savings and losses.
- Each ACO will form relationships with participating and preferred providers.
- There are still three types of ACOs: Standard, New Entrant, and High Needs Population ACOs.
- Standard: ACOs comprised of organizations with experience serving Original Medicare patients, including Medicare-only and dually eligible beneficiaries, who are aligned to an ACO through voluntary alignment or claims-based alignment. Standard ACOs may have participated in another CMS Innovation Center shared savings model and/or MSSP. New organizations composed of existing Original Medicare providers and suppliers may be created to form a Standard ACO. Either way, participating clinicians would have substantial experience serving Original Medicare beneficiaries.
- New Entrant: ACOs comprised of organizations that have not traditionally provided services to an Original Medicare population and who may rely primarily on voluntary alignment, at least in the first few performance years of participation.
- High Needs Population: ACOs that serve Original Medicare patients with complex needs, including dually eligible beneficiaries, who are aligned to an ACO through voluntary alignment or claims-based alignment.
- ACOs are identified by their Tax ID Number (TIN), and TIN splitting is still allowed, meaning some providers within an ACO may participate in the REACH program and some may not.
- The rules on model overlap remain the same – ACO REACH participating providers may not participate in most other Innovation Center Models and MSSP, however preferred providers may participate in a variety of models. But since ACO REACH participating providers are identified at a TIN-NPI level, these participating providers may participate in an overlapping model if they bill through a second TIN that is not participating in an overlapping model.
- Beneficiary attribution is calculated in the same manner for ACO REACH as it is for Direct Contracting.
- The benchmark calculations remain the same, aside from the health equity adjustments and a decreased quality withhold.
- The quality metrics remain the same for 2023 as they are in 2022 but there is a potential for adding additional quality metrics as the program progresses.
-
ACO REACH: What Has Changed From Direct Contracting?
Structure of ACOs:
-
-
- 75% of the control of the REACH ACO must be in participating providers (originally 25% in GPDC).
- 75% of participating providers within a REACH ACO must use Certified Electronic Health Records Technology (originally 50% in GPDC).
- No more than 50% of a New Entrant ACO’s participating provider roster may have experience in:
- Shared Savings Program,
- Next Generation ACO Model,
- Vermont All-Payer ACO Model,
- Comprehensive ESRD Care Model,
- Kidney Care Choices Model,
- Comprehensive Primary Care Plus Model,
- Primary Care First Model,
- Maryland Primary Care Program, or
- Pioneer ACO Model.
-
Health Equity Initiatives:
-
-
- All ACOs must develop a Health Equity Plan and report progress and outcomes to CMS.
- A benchmark adjustment ($30 PBPM) for serving the most distressed beneficiaries and a downward benchmark adjustment ($6 PBPM) for serving the least distressed beneficiaries. Review our analysis to learn more about counties that serve the most distressed populations.
-
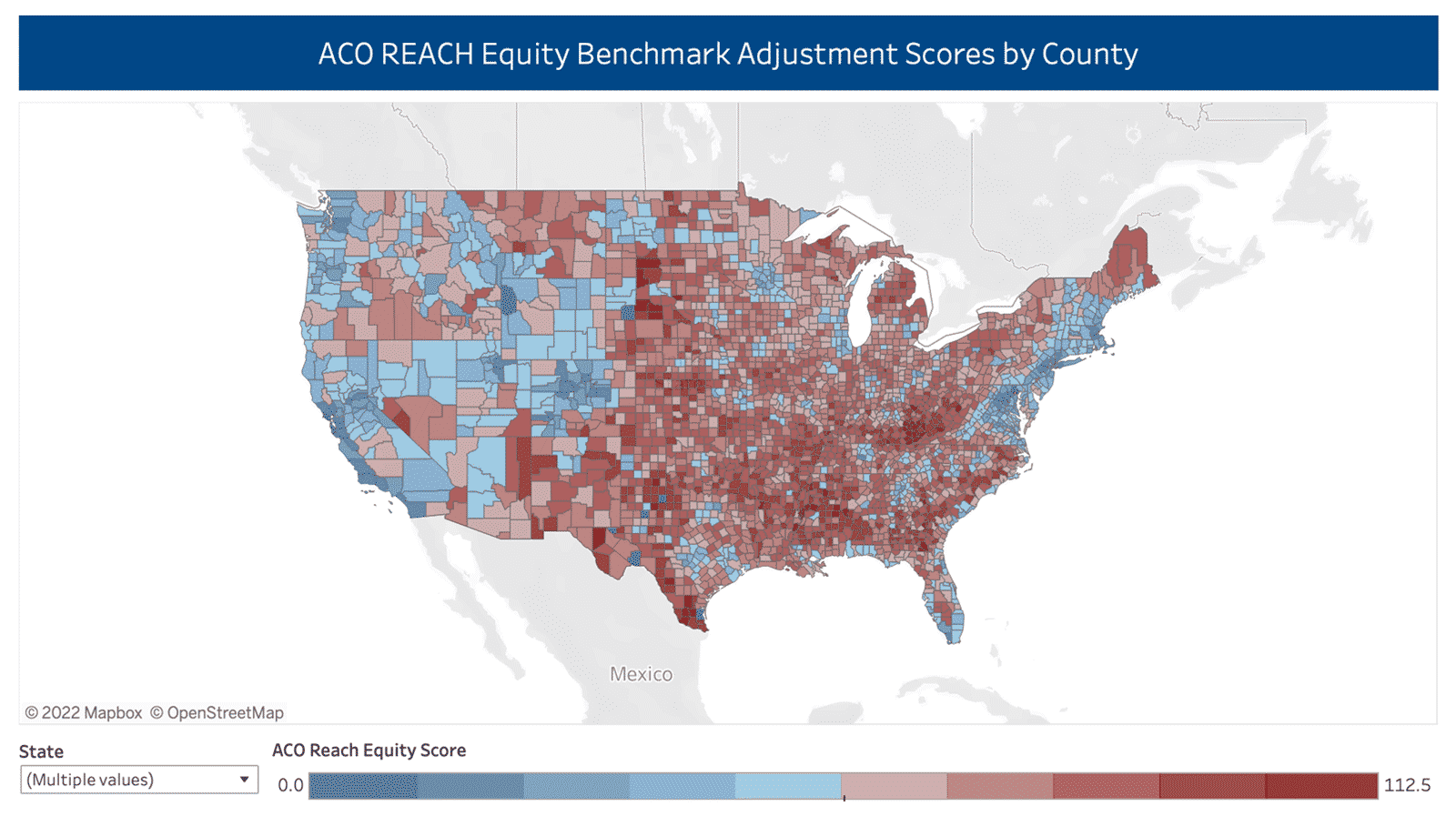
This map represents the likelihood that a beneficiary in a county will result in the $30PBPM upward benchmark adjustment (darkest red counties) or result in a $6PBPM downward adjustment (any blue county). We blended the weighted ADI score by county with the percent of dually eligible beneficiaries in that county and then deciled the scores to find the top decile and the bottom five deciles.
-
-
- All ACOs will be required to collect and report demographic information from their beneficiaries, to include race, ethnicity, language, gender identity and sexual orientation. Successful reporting will earn an ACO ten bonus points on their quality score.
- ACOs are encouraged, but not required, to collect and report social determinants of health data on their beneficiary pool.
-
Attribution/Benchmarking/Risk Adjustment
-
-
- Reduced benchmark discounts for Global risk sharing: the discount will be 3% in 2023 and 2024 and only increase to 3.5% for 2025 and 2026 (up to 5% in GPDC).
- No more than 50% of a REACH ACO’s patient base may have a given medical condition or belong to a special subset for which a targeted cost of care initiative exists.
- The quality withhold is decreased from 5% to 2% beginning in 2023.
- Stop-loss insurance points will no longer be static, but will instead be risk adjusted attachment points to help protect an ACO from excess losses based upon an individual beneficiary’s particular health situation and not an arbitrary point.
- To address coding intensity, ACO REACH will revise the 3% cap (either direction) on HCC score changes to be based on a static base year instead of a rolling year. This cap is evaluated against a risk score for the demographics of the ACO meaning that if the ACO expands and includes a population with different demographics (age, gender, dual eligibility status, disability status), the demographic factors will be taken into consideration for the 3% cap.
- $30 PBPM bonus for serving the top 10% most distressed beneficiaries and a $6 PBPM negative adjustment for serving the bottom 50% least distressed beneficiaries. Beneficiaries are ranked by taking a composite score of the Area Deprivation Index at the Census Block Group level and adding 25 points if they are dual eligible. The beneficiaries are then deciled to find the top ten and the bottom fifty percentiles.
- A High Performers Pool in which ACOs can earn extra money. Any ACOs who pass the CI/SEP (Continuous Improvement) but do not earn their entire quality withhold back will contribute the unearned portion to the High Performers Pool. ACOs who are High Performers can then earn the right to split this bonus pool on a per capita basis. The details of what constitutes a High Performer and other details will be furnished prior to 2023.
-
Data Standards/Collection/Interoperability:
-
-
- If ACOs have agreements with participating/preferred providers that involve the sharing of medical records, these programs must meet current federal interoperability standards.
- Beginning PY2023, ACOs will be required to collect and submit demographic data on their beneficiaries using either Excel or a CMS provided FHIR app.
-
Why Understanding Risk Scoring in the ACO REACH Model is Critical For Success
One major concern about the Direct Contracting model was risk scoring abuse. Read how the updated model plans to address risk scoring.
Explore with CareJourney
CareJourney is a trusted partner to dozens of ACOs and DCEs, supporting new entrants to the ACO Reach Program as well as current DCE participants looking to transition to the new program. Our current members represent over half of the participating and preferred providers in Direct Contracting, making us the leading insights provider for these new and evolving risk models.
Data remains a critical component for REACH ACOs to succeed in the program. On a financial level, benchmarking, beneficiary alignment, risk score, and quality measure metrics will allow ACOs to gauge their performance within a given model year and make any modifications to their business model or practices for better success in future years. Additionally, REACH ACOs will need to develop a data strategy to examine the demographics, social determinants of health, and health inequities within their beneficiary base and the potential beneficiaries in their service area. REACH ACOs will need to track various measures in order to report successes and outcomes back to CMS as part of their required health equity plan.
CareJourney is your partner in all of these data strategies. Stay tuned as we continue this series spotlighting different areas within the ACO REACH program where our data can help your REACH ACO not just achieve financial savings, but provide better quality healthcare to all of the beneficiaries in your service area.
For existing DCEs (and future REACH ACOs), below are some additional ways CareJourney can help:
-
-
- Model attribution to help you understand alignment volumes
- Profile your regions and providers to understand the best partners
- Simulate your benchmarks to project your performance before finalizing your rosters
- Surface opportunities for Performance Improvement using your CMS supplied claims data
-
Not ready for a meeting? Check out our resources to learn how CareJourney helps payer, provider, and pharma organizations reduce the total cost of care and improve care quality.
