Elderly beneficiaries with major comorbidities have a major impact on the healthcare landscape. Managing quality care for this population is complex and often presents financial challenges. Studies from the US Department of Health and Human Services (DHHS) show that one in four Americans have at least two chronic conditions. When beneficiaries of this population increase in age, so does the number of conditions and associated complications. As an individual’s number of conditions increase, so does their likelihood of experiencing the following outcomes:
- Mortality
- Poor functional status
- Avoidable hospitalizations
- Polypharmacy and adverse drug events
- Duplicative tests
- Conflicting medical advice including conflicting and redundant care coordination efforts
There are several reasons why improving the quality of care delivered to older adults with major comorbidities should be a priority. Multiple chronic conditions have the highest prevalence in older adults and despite making up the smallest portion of the US population, they account for the highest percentage of Medicare spend (Figure 1).1 With these factors in mind, policymakers created payment models that hold providers, on the acute and post-acute level, to a certain standard of quality to receive full CMS reimbursements. For high-need populations in a service area that are transitioning to Skilled Nursing Facilities (SNF) or other post-acute care (PAC), proper care coordination strategies must be practiced to ensure the highest-performing providers serve them, given the disproportionate impact these individuals have on cost and outcomes.1
Figure 1 below illustrates the frail/elderly population making up the smallest percentage of all patients, but contains the most high-cost patients out of all patient segments which correlate to the largest spend.
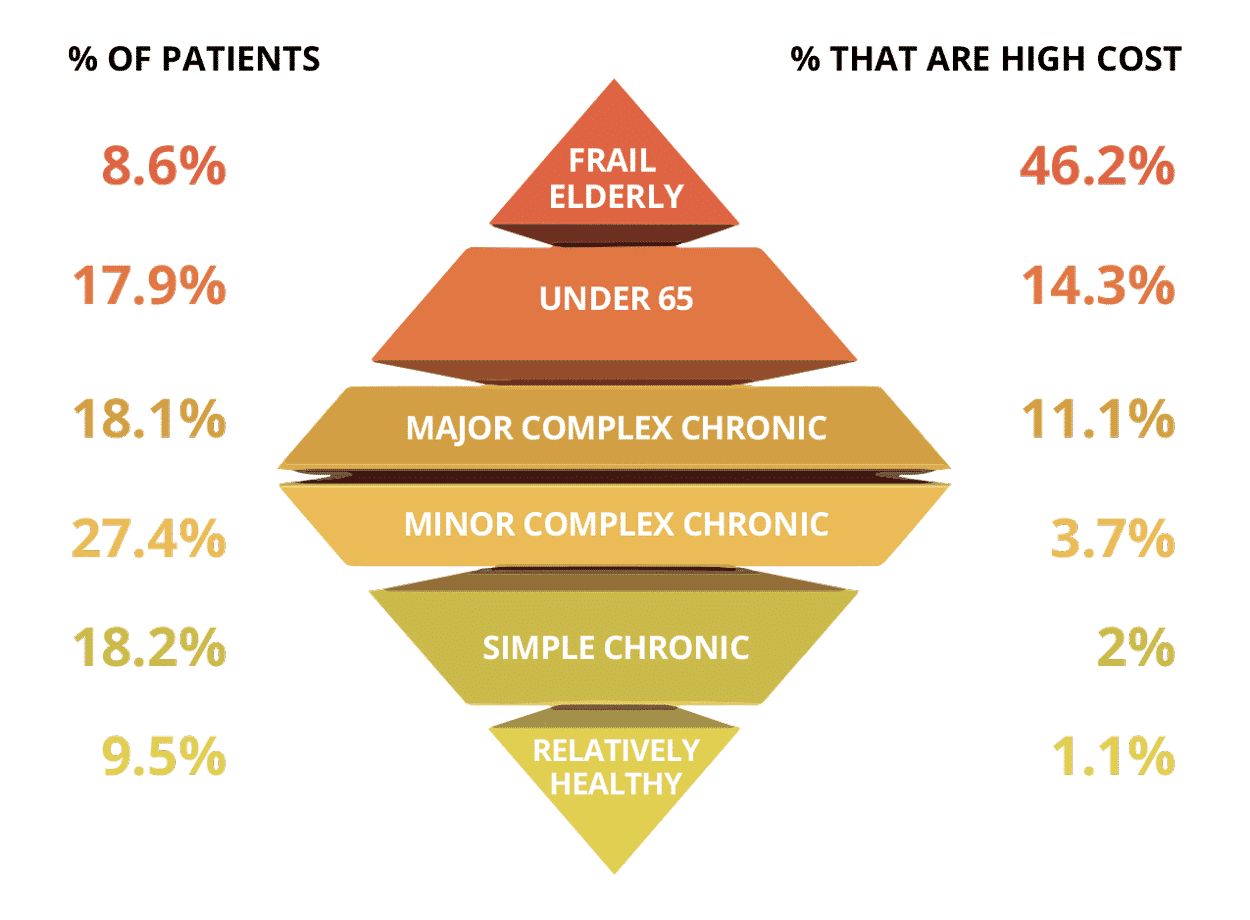
Figure 1
See PAC Utilization and Cost Data
Access our live data dashboard containing key PAC utilization metrics by site of service across California, Texas, and Florida. See data including average HCC score, readmission rate, and cost per episode across care settings.
Acute Care Transitions to Skilled Nursing Facilities
Skilled Nursing is defined by CMS as nursing and therapy care that can only be safely and effectively performed by, or under the supervision of, professionals or technical personnel.2 To qualify for these specialized services, beneficiaries must meet criteria set by CMS.
“Roughly 40% of Medicare beneficiaries are discharged to a post-acute setting, with roughly half of these to a SNF, which is a nursing home (or distinct part of a nursing home) devoted to providing skilled nursing care or rehabilitation services”.3
The goal of the providers, in the Hospital and SNF settings, is to improve the patient’s health status for a lower (less costly) level of care, and to decrease the patient’s length of stay. With these goals in mind, healthcare leaders emphasize educating staff on appropriate care-transitioning workflows and elements.
Given that discharges from acute inpatient to SNF make up 20% of all Medicare discharges, rehospitalizations from SNFs are costing CMS billions of dollars a year. Policymakers want acute and post-acute care entities to be accountable for readmission rates by provisioning reimbursements based on their ability to manage this metric. This can be a challenge for SNFs when the primary patient population consists of older adults with major comorbidities. This is why health systems and value-based care organizations are aligning with SNFs to create networks of high-performing SNFs that can encourage care coordination strategies between the hospital and SNF care settings. There is evidence that discharge to a SNF with a strong linkage to the hospital is associated with lower readmission rates.4, 5
Take California as an example of healthcare spending (Figure 2). Figure 2 below shows readmission rates (admission to hospital 30 days post-discharge) across post-acute care settings for the entire year of 2020 in California. The diagnosis related groups (DRGs) examined in the figure are three diagnoses following which readmissions are potentially avoidable per CMS:
- Coronary Bypass with major comorbidity – DRG 235
- Major Hip and Knee replacement major comorbidity- DRG 469
- Simple Pneumonia with major comorbidity – DRG 193
In one of the most populated states in terms of Medicare beneficiaries, the SNFs accumulated one of the highest number of episodes, highest number of readmission rates, and the highest amount of total allowed spend in the year.
Care Coordination Data for Beneficiaries in California with Major Comorbidities
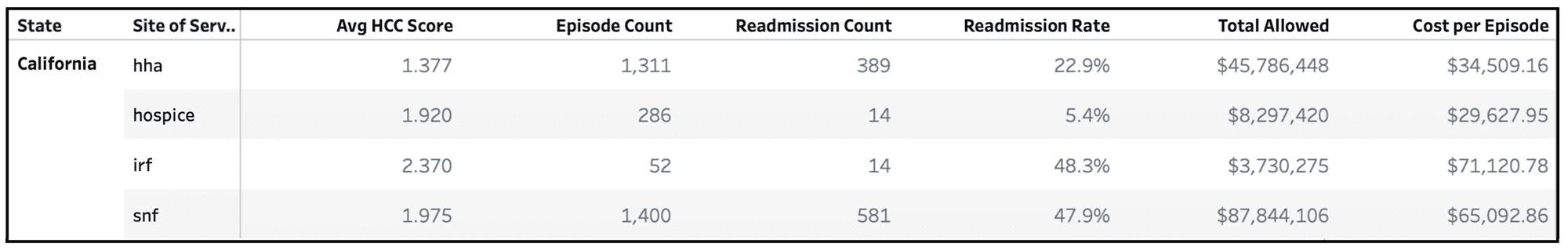
Figure 2
Fill out the form above to access our live data dashboard outlining these metrics across Texas, California, and Florida for three different diagnoses.
Patient Driven Payment Model
CMS has made changes to the way they reimburse SNFs by instituting Pay-Per-Performance Initiatives like the Patient Driven Payment Model (PDPM). The goal of this model is to deliver appropriate SNF services based on patient need rather than the volume of care provided. Due to this approach, emphasis has been placed on the assessment of patients when they are transitioned to a SNF. Assessments occur every quarter from admission and are submitted through a minimum data set (MDS) to CMS and will determine how much SNFs are reimbursed. This model challenges SNFs to provide the appropriate amount of care which will prevent over- or under-delivering therapy services.
In order to keep up with the regulations of this payment system, CareJourney has been collecting data and strategizing ways to display quality metrics around PDPM so that members are prepared to make business decisions based on quality measures that drive patient-centered care for SNFs and the management of care for high risk complex adults.
Improving Post-Acute Care Coordination to Reduce Readmissions
Reducing preventable readmissions is critical because they are associated with adverse events, higher healthcare costs and most importantly, deleterious effects on quality of life.6, 7 Care coordination strategies to reduce preventable admissions can include:
Patient interventions: Conduct early risk screening to identify patients who warrant intensified post-discharge support services, promoting follow-up with primary or specialty care, patient education, optimized medication management, post-discharge phone calls, and transition coaches.8

Enhanced communication between care settings: Establish a clinical liaison at hospitals and SNFs to quickly communicate unexpected changes in patient status. Hospital liaisons can share the patient’s care plan with the SNF for proper discharge planning and post-discharge follow-up.
Frequent readmission review: Make providers aware of high-risk beneficiaries in order to strategize an integrated care plan that ensures a patient will not readmit to the hospital.
Shared clinical pathways: Embed higher level clinical services in SNF partners, including via telemedicine, in order to handoff from the SNF back to the community care team.
How CareJourney Can Help
Using a nationwide FFS claims dataset, CareJourney enables its members to assess the SNFs that belong in their network by providing cost and quality metrics for all facilities in the nation. Users are able to view which SNFs are receiving hospital referrals as well as compare the performance of SNFs across several quality measures like length of stay and readmission rates.
At a granular level, users can see detailed metrics describing the rendered care before, during, and after a SNF admission, simplifying network and routing decisions. Using the ability to combine claims data, open data, and member data together, CareJourney gives its members a complete profile for SNF providers with the goal of producing healthcare solutions. Enhancing a network of high performing SNFs to account for beneficiaries with major comorbidities can improve outcomes and reduce spend on this complex population.
- https://carejourney.com/medicare-home-health-beneficiaries/
- Skilled Nursing Facility (SNF) Care.” SNF Care Coverage, CMS, https://www.medicare.gov/coverage/skilled-nursing-facility-snf-care.
- Agency for Healthcare Research and Quality HCUPnet. 2009. [cited 2009 July 21]; Available from: hcupnet.ahrq.gov
- Hospital-Skilled Nursing Facility Referral Linkage Reduces Readmission Rates Among Medicare Patients Receiving Major Surgery, Andrew J. Schoenfeld, Xuan Zhang, David C. Grabowski, Vincent Mor, Joel S. Weissman, Momotazur Rahman
- Effect of Hospital–SNF Referral Linkages on Rehospitalization, Momotazur Rahman, Andrew D Foster, David C Grabowski, Jacqueline S Zinn, Vincent Mor Health Serv Res. 2013 Dec; 48(6 Pt 1): 1898–1919. Published online 2013 Oct 17. doi: 10.1111/1475-6773.12112
- Hoyer, E.H., Brotman, D.J., Apfel, A. et al. Improving Outcomes After Hospitalization: A Prospective Observational Multicenter Evaluation of Care Coordination Strategies for Reducing 30-Day Readmissions to Maryland Hospitals. J GEN INTERN MED 33, 621–627 (2018). https://doi.org/10.1007/s11606-017-4218-4
- Identifying potentially preventable emergency department visits by nursing home residents in the United States, Robert E. Burke, Sean P. Rooks, Cari Levy, Robert Schwartz, Adit A. GindeJ Am Med Dir Assoc. Author manuscript; available in PMC 2016 May 1.Published in final edited form as: J Am Med Dir Assoc. 2015 May 1; 16(5): 395–399. Published online 2015 Feb 18. doi: 10.1016/j.jamda.2015.01.076
- Association between Acute Care and Critical Illness Hospitalization and Cognitive Function in Older Adults, William J. Ehlenbach, Catherine L. Hough, Paul K. Crane, Sebastien JPA Haneuse, Shannon S. Carson, J. Randall Curtis, Eric B. Larson
JAMA. Author manuscript; available in PMC 2010 Sep 22.Published in final edited form as: JAMA. 2010 Feb 24; 303(8): 763–770. doi: 10.1001/jama.2010.167 - Hoyer, E.H., Brotman, D.J., Apfel, A. et al. Improving Outcomes After Hospitalization: A Prospective Observational Multicenter Evaluation of Care Coordination Strategies for Reducing 30-Day Readmissions to Maryland Hospitals. J GEN INTERN MED 33, 621–627 (2018). https://doi.org/10.1007/s11606-017-4218-4
