Double Clicking into Performance: How Data Across ACOs, Providers, and Patients Drives Better Outcomes
By Carl Vidrine and Blair Mohney
December 12, 2024
Explore how a management services organization (MSO) leveraged multi-layered data to strengthen their value-based care strategy, mitigate risk, and improve patient outcomes.
As we gear up for Performance Year (PY) 2025, risk-based Accountable Care Organizations (ACOs) are juggling a lot. Earlier this year, we described the delicate balancing act of reviewing PY 2023 results, performing in PY 2024 for an accountable population, and strategizing for PY 2025.
The Balancing Act
As we close out 2024, ACOs are pivoting more heavily towards preparing for 2025 and planning impactful interventions to drive savings.
Yet, in reflecting across PY 2023 results as well as the broader PY 2024 year, we’ve seen one approach serve a lot of organizations well: successful ACOs often weave together a performance narrative for their entire organization, looking across all physicians, evaluating the segments of care they manage, and drilling down to specific patients.
While not novel, this unified, top to bottom performance assessment allows organizations to identify and act on impactful levers, track success, and ensure value.

In a two-part blog post, we’ll outline our thoughts on this approach and its impact. To start, we will demonstrate this segmented performance approach with a sample ACO considering opportunities for data analytics to underpin sound decision-making.
In part two of the series, we will dive into PY ’23 results, outlining trends in shared savings to inform PY ‘25.
The Case for Multi-Layered Performance Data
To demonstrate the value of a multi-layered performance approach allowing organizations to identify levers that move the needle for their patients and bottom lines, we will use the story of a blinded risk entity based on real CareJourney data.
Meet Our Risk Entity
A medium-sized Managed Services Organization (MSO) is exploring the acquisition of an Accountable Care Organization (ACO). This MSO sought to integrate the ACO’s practices into their value-based care (VBC) product portfolio.
However, this was not a binary decision. Instead, the MSO looked to allocate the acquired practices across various high-risk and low-risk VBC models. Success hinged on understanding individual practice performance within the ACO contracts to inform the correct placement.
Their Challenge: Uncovering Performance Insights and Taking Action
Specifically, this organization sought to:
- Identify which practices could sustain high-risk, high-reward payment models
- Recognize underperforming practices and minimize financial exposure through lower-risk models
- Guide practices toward success based on their unique areas of opportunity across all risk models
The organization chose a data strategy with high-level contract insights, granular performance of individual practices, and actionable segmentation to identify improvement areas.
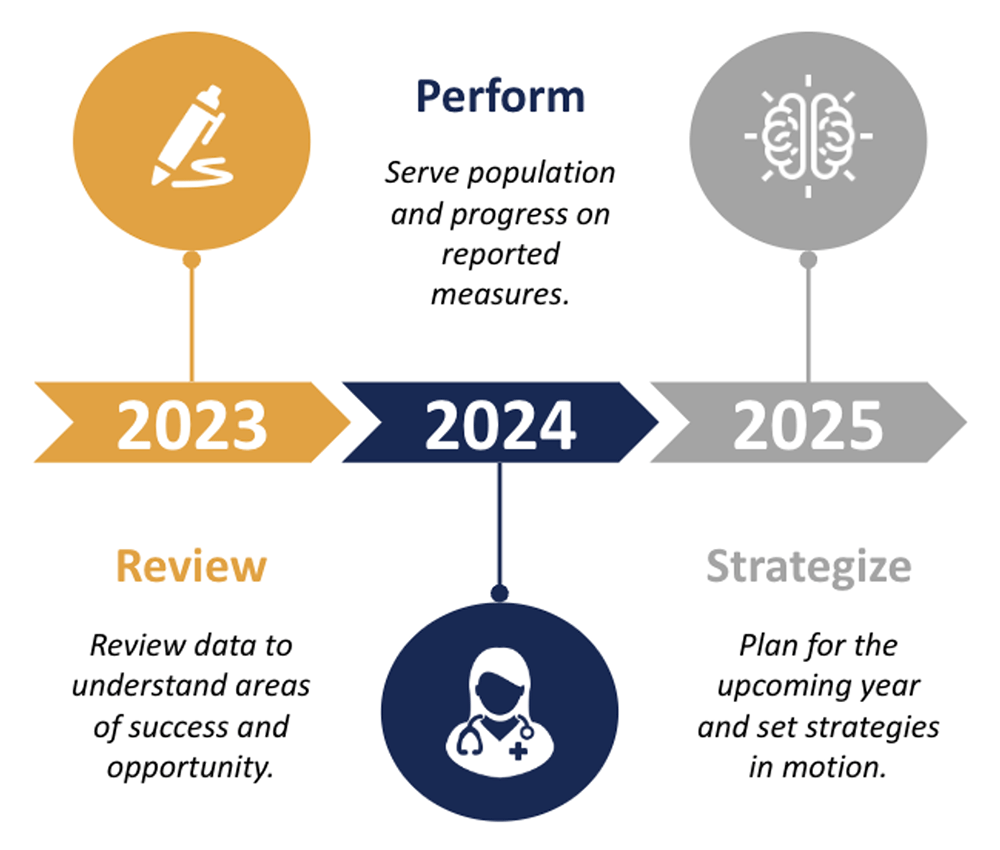
The ACO Contract Level: Understanding Financial Modeling
To outline their approach, the organization started with financial modeling to evaluate their acquisition. They created performance models along a spectrum of measures such as identifying anticipated benchmarks, patient attribution, and projected performance based on historical trends. Across these models, the organization clearly saw:
- High-performing practices that drove the ACO success
- Practices operating at breakeven levels
- Underperforming practices that posed a potential financial risk
Sample CareJourney modeling contract performance – identifying anticipated performance across contract scenarios.
With this contract modeling, the organization slated high-performing practices for high-risk, high-reward products and underperforming practices for upside-only models, minimizing downside financial exposure.
Many organizations stop here, missing opportunities to support underperforming practices and those hovering around break-even levels with the data to help them improve. To optimize the performance of these groups, we unpacked the root causes of their performance and ways in which to improve.
The Provider Level: Discovering Care and Performance Gaps
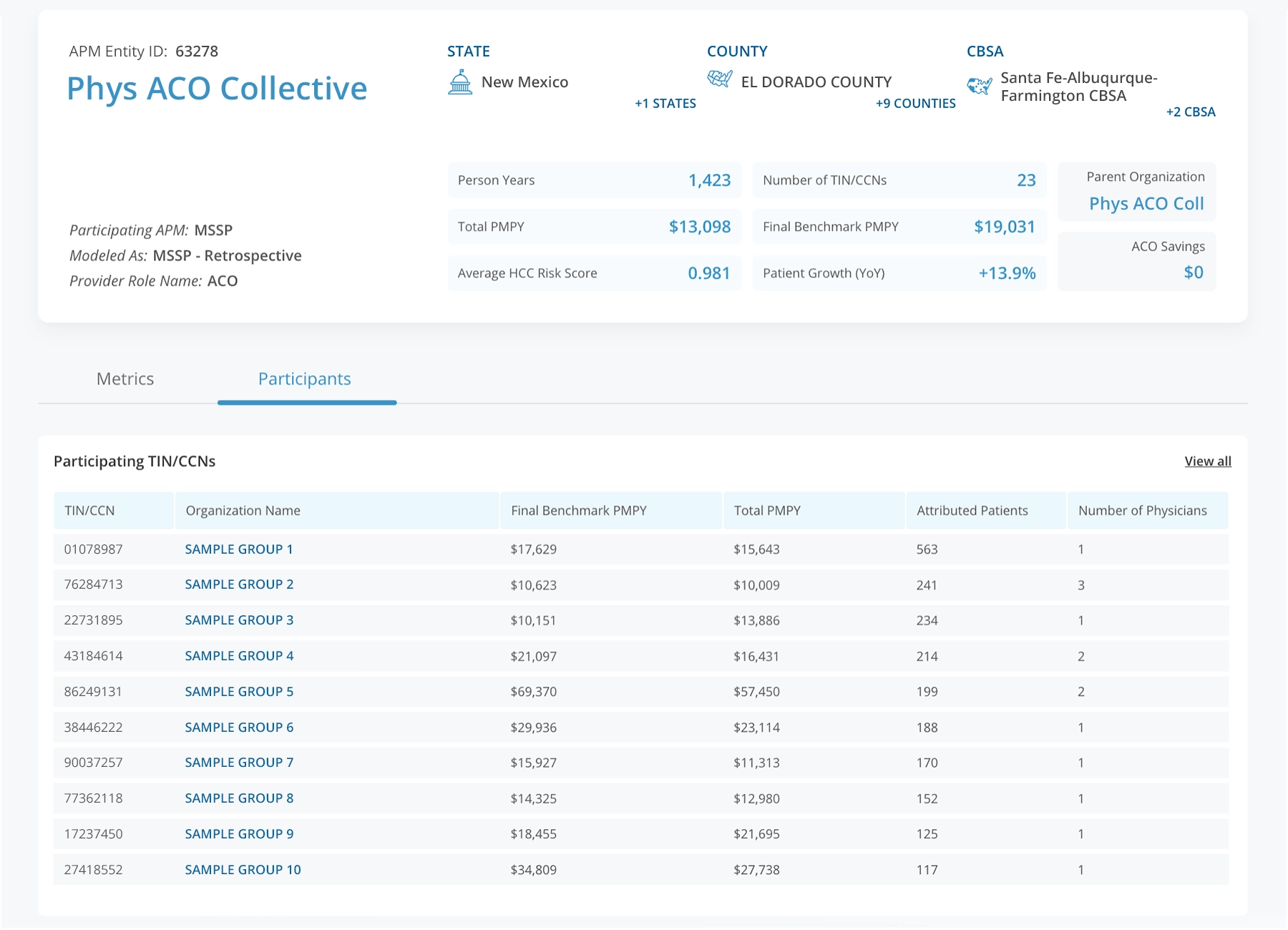
This brings us to a second layer of performance. Armed with these insights, the organization sought to develop a targeted integration strategy supporting these practices to further improve their performance. Their strategy centered around primary care providers (PCPs), the cornerstone of effective care coordination. The ability to optimize PCP performance not only has a significant impact on overall financial success but also improves patient outcomes.
By identifying performance gaps, the organization can strategically target interventions to enhance care delivery and optimize savings potential. Identifying performance gaps is only part of the challenge. Creating plans to close these gaps requires data that unpacks the reasons for these gaps. To successfully uncover the “why,” ACOs need to efficiently profile practice groups and individual physicians across the segments of care they manage.
Sample CareJourney provider performance profile – drilling into actionable segments of care.
In the instance above, the organization saw Dr. Davis underperform relative to benchmarks, presenting clear opportunities for improvement. For Dr. Davis, their overall performance is strong, but there’s significant room for improvement within their frail elderly population. This provider could uncover approximately $200,000 in potential savings by better addressing the needs of this high-risk group.
While this unpacks an area of improvement, it still doesn’t drive action. The question becomes: how can we make a difference?
The Patient Level: Identifying High-risk Patients for Interventions
The answer lies in another layer of data: identifying high-risk patients, activating a team to support them, and developing targeted interventions.
Upon analyzing Dr. Davis’ patient panel in our case study, we discovered nine frail elderly patients with significant care needs. Three of these patients have incurred expenditures this year that are double those of last year, while one patient’s costs have tripled. These trends indicate a pressing need to engage these patients proactively as their healthcare utilization increases rapidly.
A closer look at individual patient profiles provides even more actionable insights. For instance, one patient is managing several serious chronic conditions and has visited the emergency department 15 times in the past six months. Additionally, this patient is not enrolled in Part D, creating a critical opportunity for the care management team to intervene. By addressing this gap, organizations can better coordinate care, reduce avoidable utilization, and improve outcomes.

Sample CareJourney patient profile – highlighting patients for action.
With this performance layer, near real-time data—available within just three days of an event— is critical, enabling swift intervention to address emerging issues.
The Impact: A Complete Strategy From ACO- to Patient-level
A complete strategy connects modeled ACO performance down to the patient level for interventions. With these data-driven insights, the MSO was able to:
- Strengthen their negotiation position in demonstrating their value for the acquired ACO
- Tailor their value proposition to the specific needs and performance levels of individual practices
- Mitigate risk by correctly aligning practices to high-risk or upside-only models
- Most importantly, best support patients by identifying specific areas where interventions can quickly support patient needs and improve these patients’ outcomes. This not only enhanced our MCO’s acquisition strategy but also optimized its value-based care offerings, ensuring sustainable growth and improved financial and patient outcomes across the portfolio.
The right data partner equips organizations with the right data strategy to leverage early indicators, historical trends, and comprehensive benchmarking to drive smarter, more impactful decisions across all levels of performance (ACO, systems, provider groups, episodes of care, and patients). This reduces the administrative burden and allows organizations to focus on what matters most: delivering high-quality care.
As a follow up to this post, stay tuned to unpack how this multi-layered, episodic data approach sheds light on PY 2023 results and unearths efforts that contributed to shared savings.
About CareJourney By Arcadia
Since its founding in 2014, CareJourney has believed in the importance of our nation’s transition to value-based care but recognized the absence of a reliable “operating manual” for delivering on its promise of better quality at lower costs. That’s why CareJourney’s mission is to empower organizations and the people they serve with open, clinically relevant analytics and insights to optimize healthcare journeys.
In 2024, CareJourney was acquired by Arcadia, blending clinically relevant cost, quality, and benchmark data into Arcadia’s next-generation healthcare data platform and workflow tools. Together, we enable organizations to grow high-performing networks, accelerate digital transformation, and achieve success in value-based care at speed, scale, and sophistication.