Chronic Kidney Disease: Patterns in Racial Health Inequity in CKD Diagnosis
Written in partnership with Carenostics
By Soleil Valentin, Nate Smith, Aneesh Chopra, Bharat Rao
November 28, 2023
In our previous blog we described the gaps in the diagnosis of Chronic Kidney Disease (CKD). In this blog we highlight that, while the negative impacts of underdiagnosis within the overall population are shocking, the disparities that exist in vulnerable, historically-disadvantaged populations are even more alarming. Specifically, African Americans have higher CKD prevalence and higher kidney disease mortality compared to non-Hispanic White Americans. African Americans are 300% more likely to suffer from kidney failure. While only one in eight Americans is African American, one-third of kidney failures happen among this demographic.1
In addition to elevated kidney disease morbidity and mortality, African Americans face a greater underdiagnosis problem than other racial groups. This is partly due to a much-discussed racial component in historical eGFR test scoring, as well as a variety of socio-economic issues, including fewer PCP appointments, lower medical insurance enrollment, reduced healthcare access, reduced testing, and systemic racial biases.2 The focus of this blog is not to quantify the relative contribution of these factors to the underdiagnosis of CKD among African Americans. Our focus is to propose a method to measure the degree of health inequity in CKD underdiagnosis, and illustrate that this health inequity metric can be useful in identifying geographic areas where closing the equity gap can have the largest impact on patient lives.
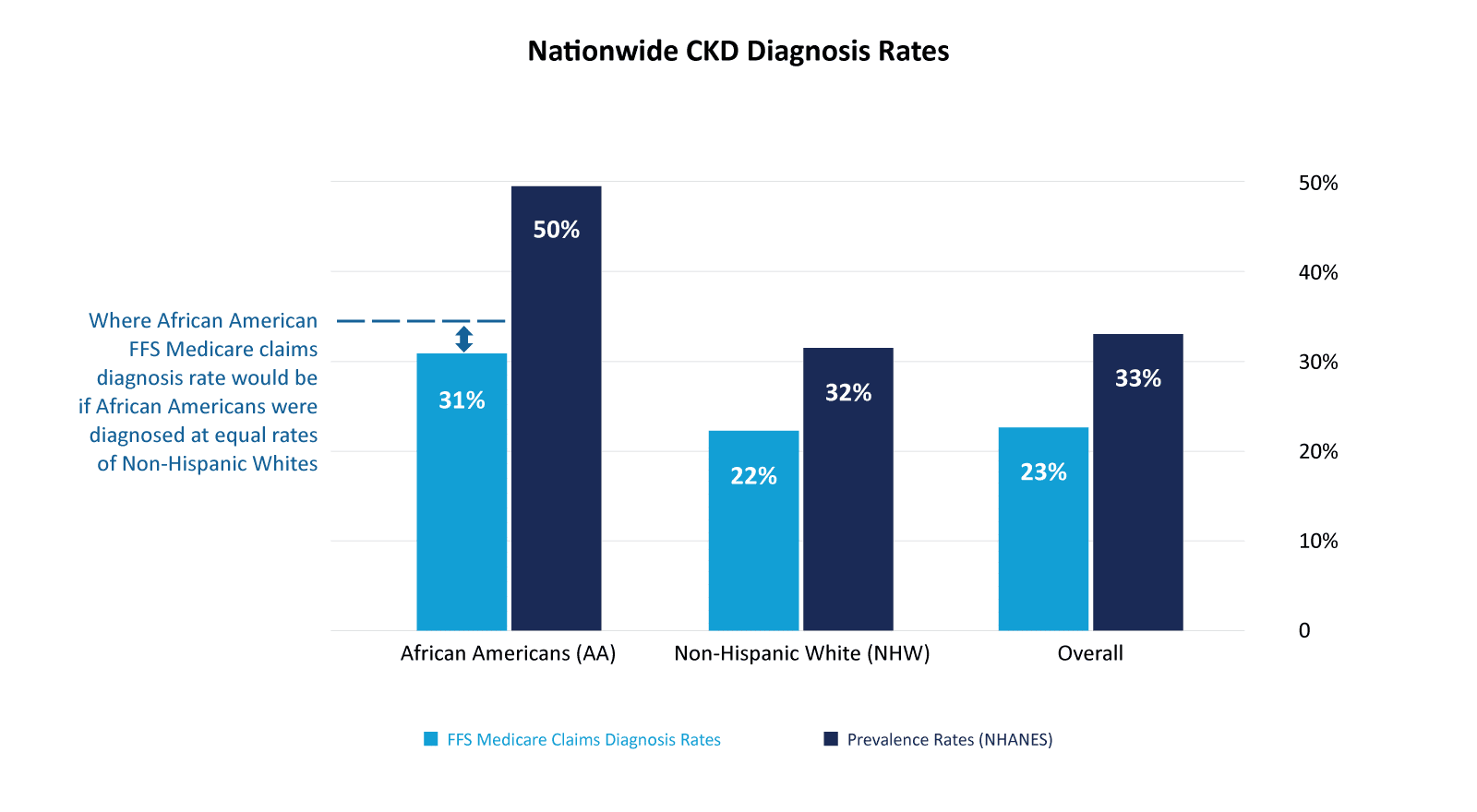
Promoting and improving health equity are core values at both CareJouney and Carenostics. We are continuing our partnership to further explore and quantify the health equity issues and care gaps in the diagnosis and treatment of CKD. CareJourney’s extensive CMS claims dataset of over 200M+ longitudinal claim records enables the examination of health equity patterns among the US senior population (above the age of 65), and assessment of the role of race and health equity in the gaps in CKD diagnosis. According to the National Health and Nutrition Examination Survey (NHANES), the prevalence of CKD among the African American senior population is 50%.3 However, our analysis of 2021 Fee For Service (FFS) claims data shows that the diagnosis rate for the African American senior population is only 31%, meaning that an estimated 19%, or approximately 1 million African Americans over the age of 65, are likely to have undiagnosed CKD. CKD can be diagnosed at an early stage with simple blood and urine tests, and new treatments are available that can dramatically slow disease progression, delay/prevent dialysis, reduce treatment costs and save lives. However, the level of under-diagnosis suggests that these simple diagnostic tests are not administered in a racially equitable manner, contributing to delayed treatment and worse outcomes in these vulnerable subpopulations.
Note: Senior population defined as over the age of 65.
Data: Carenostics analysis of CareJourney traditional FFS Medicare claims data of the senior population.
NHANES Data: CKD status was determined by single measurements of kidney function (eGFR and albuminuria)
Given this understanding of the difference in CKD prevalence by race among seniors, we looked into the diagnosis ratio of African Americans (AA; 31%/50% = 0.620) and compared it to the diagnosis ratio of non-Hispanic Whites (NHW; 22%/32% = 0.688) Americans. We calculate a new metric, the Diagnostic Equity Ratio, that compares the diagnosis ratios of African Americans and Non-Hispanic White Americans. If the rate of diagnosis matches the underlying prevalence rate, the Diagnostic Equity Ratio is 1.00. Ratios below 1.00 indicate AA diagnosis rates below the equitable rates. For example, nationally the diagnostic equity ratio is .90 (0.620 / 0.688). This implies that, in addition to “regular” underdiagnosis that impacts all races, ~58,000 African American Medicare beneficiaries are currently undiagnosed due to health inequities.
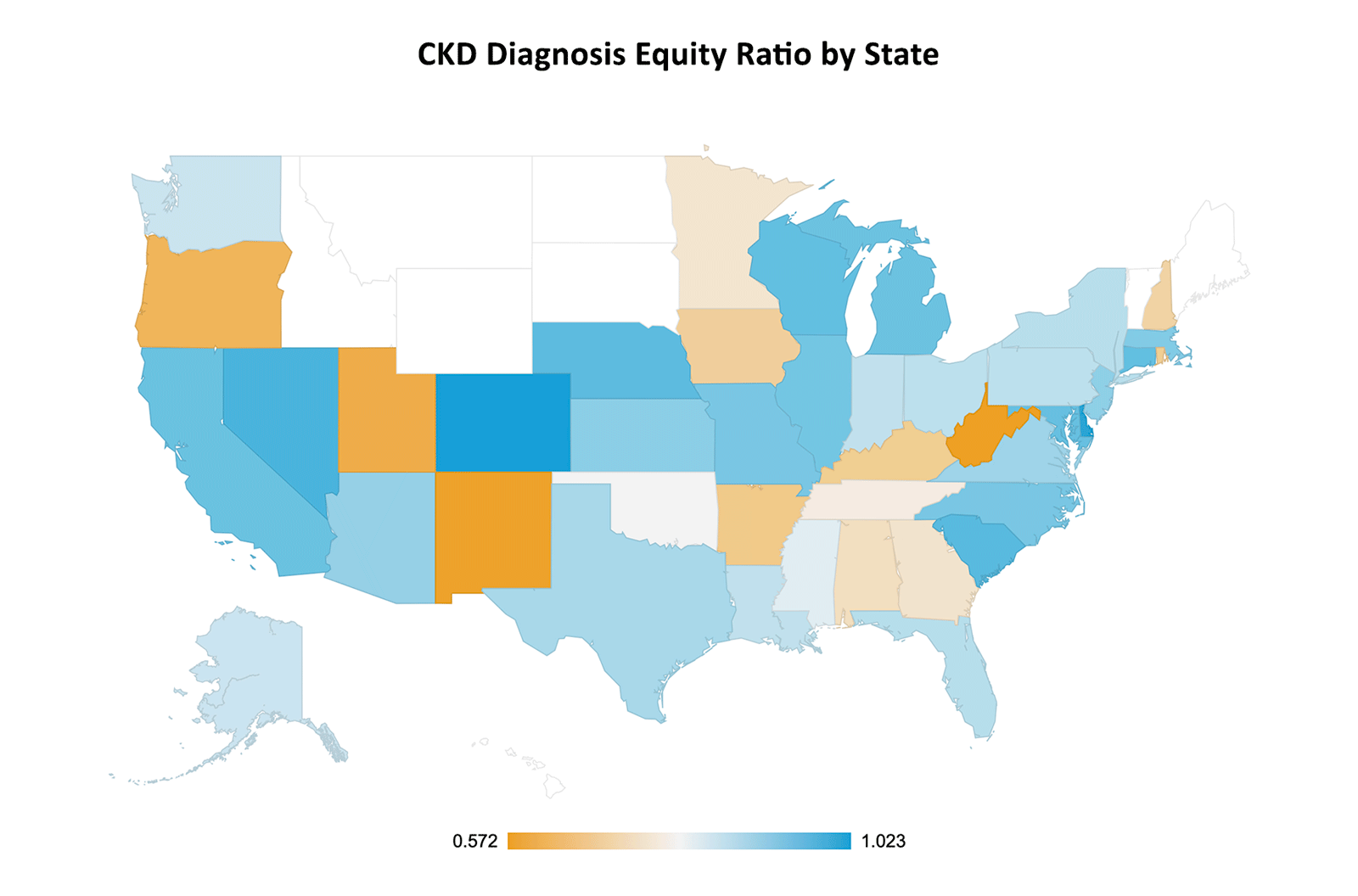
Note: States shown in white had very few African Americans diagnosed with CKD
When examining the Diagnostic Equity Ratio for the senior populations by state, we found wide variability. The four states with the highest Diagnostic Equity Ratio (all near 1.00, indicating equity in diagnosis) are Colorado, Delaware, Nevada, and South Carolina. The states with the lowest Diagnosis Equity Ratio (indicating a high level of inequality in diagnosing chronic kidney disease) are West Virginia, New Mexico, Utah, and Oregon. However, while these states have the lowest diagnosis equity ratio, they also have relatively small African American populations.
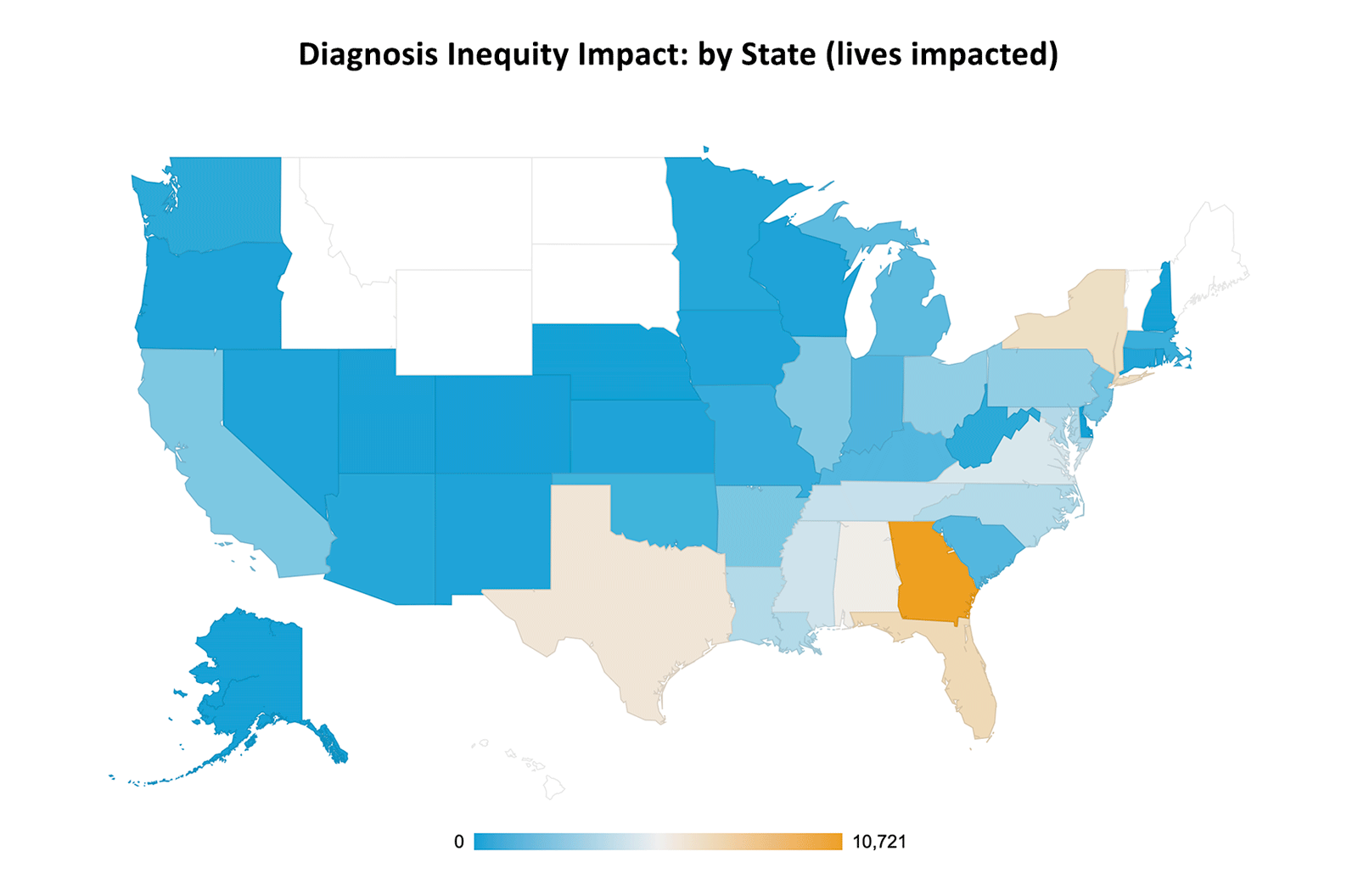
Next we take each state’s African American population size into account and look at the number of patients that would be diagnosed if only the equity gap were to be closed. When doing this, Georgia is the state where closing the inequality gap would impact the most people: we estimate that equitable diagnosis in GA would result in over 10,000 additional African American seniors being diagnosed with CKD. Florida, New York and Texas are three additional states where closing the diagnosis equity gap would improve the lives of thousands of African American seniors. However, this is just the equity impact. The map below shows the number of African American patients needing a CKD diagnosis to close the equity gap. The true problem is worse, because even with equitable diagnosis, CKD is dramatically underdiagnosed in all populations, as we outlined in our previous blog.
Solving the undertreatment problem for CKD first requires identifying the undiagnosed CKD population. Artificial Intelligence (AI) and Machine Learning (ML) have the potential to dramatically transform the costs and outcomes of CKD by identifying novel markers of risk, monitoring healthy individuals, and predicting disease in undiagnosed patients (enabling proactive clinician intervention). However, a recent and highly publicized healthcare study by Obermeyer (2019) found that an ML algorithm used nationwide to identify millions of patients for coordinated health care management programs prioritized healthier non-Hispanic White patients over significantly sicker African-American patients.4 Research has shown that AI and ML methods designed without equity in mind can not only perpetuate existing disparities, but also exacerbate them.5
A more thoughtful approach to AI has the potential to solve this issue. Carenostics has been working on developing AI solutions that address the health equity gap, working closely with our advisor and recognized expert in the field of bias in AI, Professor Rayid Ghani, Distinguished Professor of Computer Science and Public Policy at Carnegie Mellon University. Prof Ghani, who has spent his career pioneering the development of AI & ML methods to solve high-impact social good and public policy problems in a fair and equitable way, remarked that “any approach that addresses the problem of underdiagnosis in underserved populations must account and adjust for the underlying biases in clinical care and healthcare data.” Carenostics has worked with Hackensack Medical Center to develop an award-winning (Bio-IT Innovation Award 2023 recipient,6 Digital Health Hub Foundation “Best Use of AI in Health Tech” Rising Star Winner7) AI solution that has demonstrated significant increase in diagnosis of undiagnosed CKD patients.
Solving the complex AI and bias-adjustment issues of CKD has the potential to get patients on guideline-directed medical therapy, significantly slow progression of this deadly disease for millions of Americans, prevent cardiovascular complications, save thousands of dollars in avoidable medical costs per patient per year, and save lives, regardless of race, and can help address health disparities in diagnosis, treatment, and outcomes.
Key Takeaways
- CareJourney’s CMS dataset of 200M+ longitudinal claim records is a vital resource for analyses of health equity patterns among the US senior population and examinations of the role of race and equity in health care gaps.
- African Americans are 300% more likely to suffer from kidney failure compared to non-Hispanic White Americans.
- The diagnosis rate for CKD among African American seniors is 31%, while the NHANES prevalence of CKD among this population is 50% suggesting a severe underdiagnosis problem.
- Disparities in current CKD diagnosis exist between African Americans and non-Hispanic White Americans, indicating a lack of equity in the healthcare system that varies by state.
- The number of lives that can be impacted by diagnosis equity-focused initiatives in each state varies based on diagnosis inequity and AA population.
- Artificial Intelligence (AI) and Machine Learning (ML) methods that account for underlying biases in clinical care have the potential to improve CKD outcomes by identifying undiagnosed patients while addressing healthcare inequality that is seen today.
- Assari, S. (2015, December 12). Racial disparities in chronic kidney diseases in the United States; a pressing Public Health Challenge with social, behavioral and medical causes. Journal of nephropharmacology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5297505
- https://www.pfizer.com/news/articles/health_disparities_among_african_americans
- U.S. Department of Health and Human Services. (n.d.-a). Annual data report. National Institute of Diabetes and Digestive and Kidney Diseases.Table 2.2.
https://usrds-adr.niddk.nih.gov/2022/chronic-kidney-disease/2-identification-and-care-of-patients-with-ckd - Obermeyer, Ziad, et al. “Dissecting Racial Bias in an Algorithm Used to Manage the Health of Populations.” Yearbook of Paediatric Endocrinology, 25 Oct. 2019, https://doi.org/10.1530/ey.17.12.7.
- Shanklin, R., Samorani, M., Harris, S., & Santoro, M. A. (2022). Ethical redress of racial inequities in AI: Lessons from decoupling machine learning from optimization in medical appointment scheduling. Philosophy & technology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9584259
- BIO IT World names 2023 innovative practices winners. Bio-IT World. (n.d.). https://www.bio-itworld.com/news/2023/04/19/bio-it-world-names-2023-innovative-practices-winners
- Health Foundation Hub. 2023 Finalists. (2023). https://www.digitalhealthhub.org/awards/2023/finalists
