Chronic Kidney Disease: The Silent Epidemic of the United States
By Kanishka Rao, Nate Smith, Soleil Valentin
July 5, 2023
Chronic kidney disease (CKD) is a condition characterized by the gradual loss of kidney function over time1 and is the eighth leading cause of death in the US.2 This widespread condition affects approximately 1 in 7 adults (more than 37 million people) and an estimated 38% of US seniors.3 Of these affected patients, it has been estimated that nearly 40% are in Stage 3 or higher where pharmaceutical intervention, as recommended by the gold-standard KDIGO guideline,4 can have a profound impact in delaying progression to kidney failure.
Despite this high prevalence, the National Kidney Foundation (NKF) estimates that 80% of CKD cases are currently undiagnosed and undertreated.5 Leaving CKD patients undiagnosed and untreated results in significant health and cost implications as it progresses further from early stage stage 3 CKD to end stage kidney disease, a deadly stage with a three-year survival of only 56%, requiring dialysis or transplant.6
Recent targeted pharmaceutical interventions have been shown to improve outcomes for patients with early stage CKD, particularly those with complicating co-morbidities. For example, for CKD patients with diabetes, treatment with SGLT2 inhibitors has been shown to delay end-stage kidney disease (ESKD) by 15 to 25 years.7 These are augmented by recent groundbreaking CKD therapies, such as nonsteroidal MRAs, which have shown a sustained decline in severity of kidney disease, slowed progression of at least 50% of patients to ESKD, and reduced death from renal or cardiovascular causes.9 Unfortunately, despite these advances, CKD remains a significant issue due to gaps in diagnosis and treatment, accounting for about one-quarter of total Medicare FFS spending, at over $75 billion.6
To help explore and address this issue, Carenostics and CareJourney have partnered to investigate and identify solutions to the gaps in the diagnosis and treatment of CKD. Leveraging CareJourney’s CMS claims dataset of over 200M+ longitudinal claim records, we analyzed diagnosis and treatment patterns among the US senior population (above the age of 65). Our analysis of 2021 Fee-for-Service (FFS) claims data reveals that the diagnosis rate for the Medicare population is only 23%, compared to 38% that the CDC estimates to be the true prevalence rate in the senior population.* This indicates that up to 15% of US seniors have undiagnosed CKD (approximately 8.5 million US seniors).
* Due to the impacts of the covid pandemic on decreased utilization of care during the reference period, it is likely that the absolute discrepancy is overstated, but still directionally accurate.
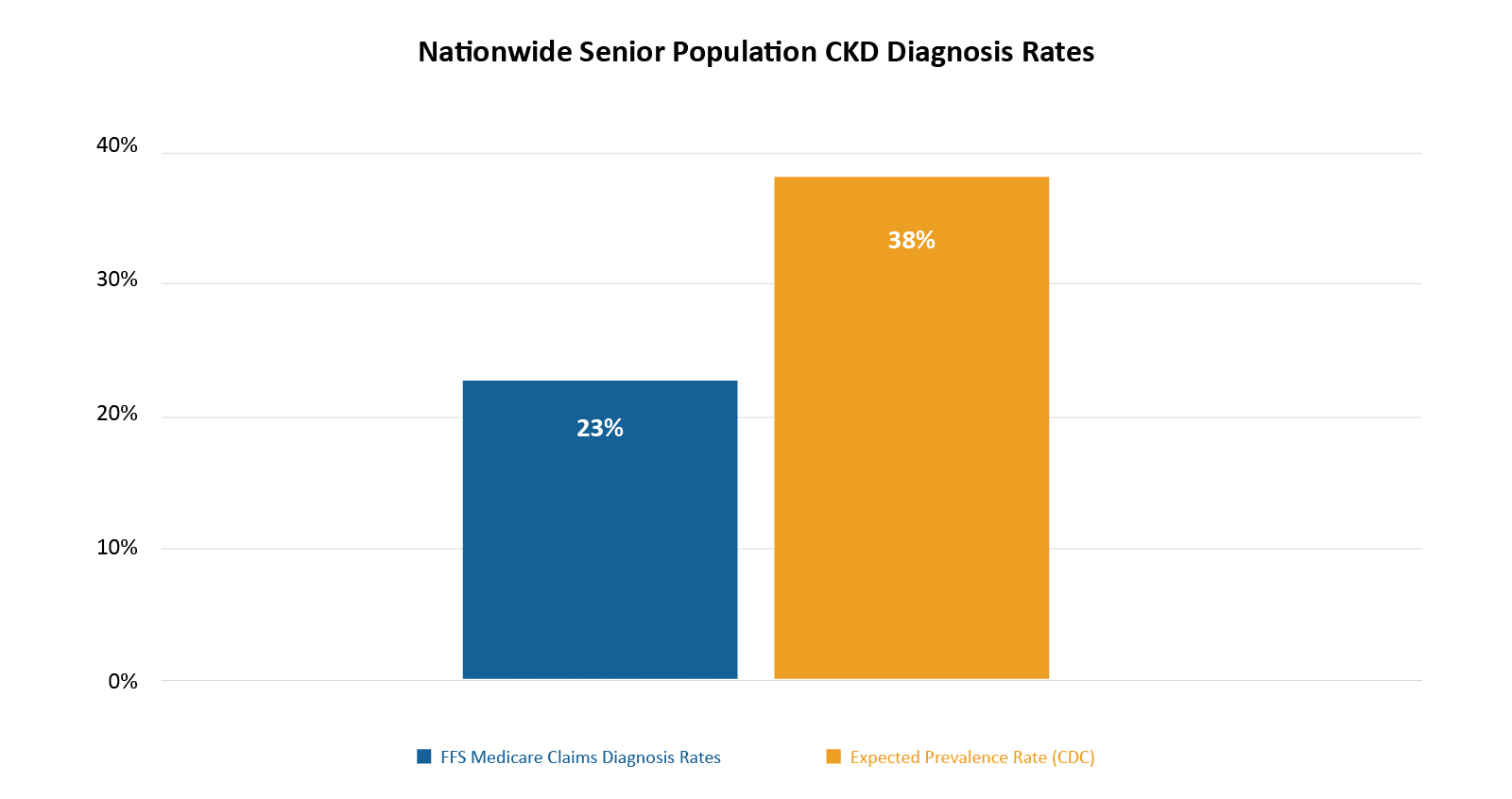
Note: Senior population defined as over the age of 65.
Data: Carenostics analytics of CareJourney transitional Medicare claims data of the senior population.
Furthermore, even for patients diagnosed with CKD, there is evidence of undertreatment. For example, despite strong evidence on improved outcomes from SGLT2 inhibitors for CKD patients with diabetes,7 our analysis shows that only 16.8% of seniors diagnosed with CKD and diabetes have been shown to take this medication, and an even smaller number of patients are taking the newer nonsteroidal MRA inhibitors, leading to potential worsening outcomes for millions of patients.
These gaps in care, stacked on top of the underdiagnosis described previously, can lead to the worsening of outcomes and rapid progression of disease. If these gaps in care are closed and patients are identified, diagnosed, and treated properly, leveraging well-defined therapeutic guidelines,4 could be prescribed which slow disease progression and reduce needless suffering and costs.2 In a recent collaboration with a large healthcare organization, we were able to demonstrate that, by mining healthcare records and applying AI techniques to generate smart alerts, we were able to identify over 50% of the estimated undiagnosed CKD patients, and further were able to improve testing and clinician activation by over 50%. Through such solutions, we can begin to close these gaps, and improve patient outcomes and quality of care for patients while substantially reducing cost to the healthcare system. This represents an immense opportunity for providers, payers (including Medicare), and pharmaceutical companies to identify patients who can benefit from these guideline-directed medical therapy. In a future blog, we will look more closely into specific areas of health inequity in relation to diagnosis and treatment.
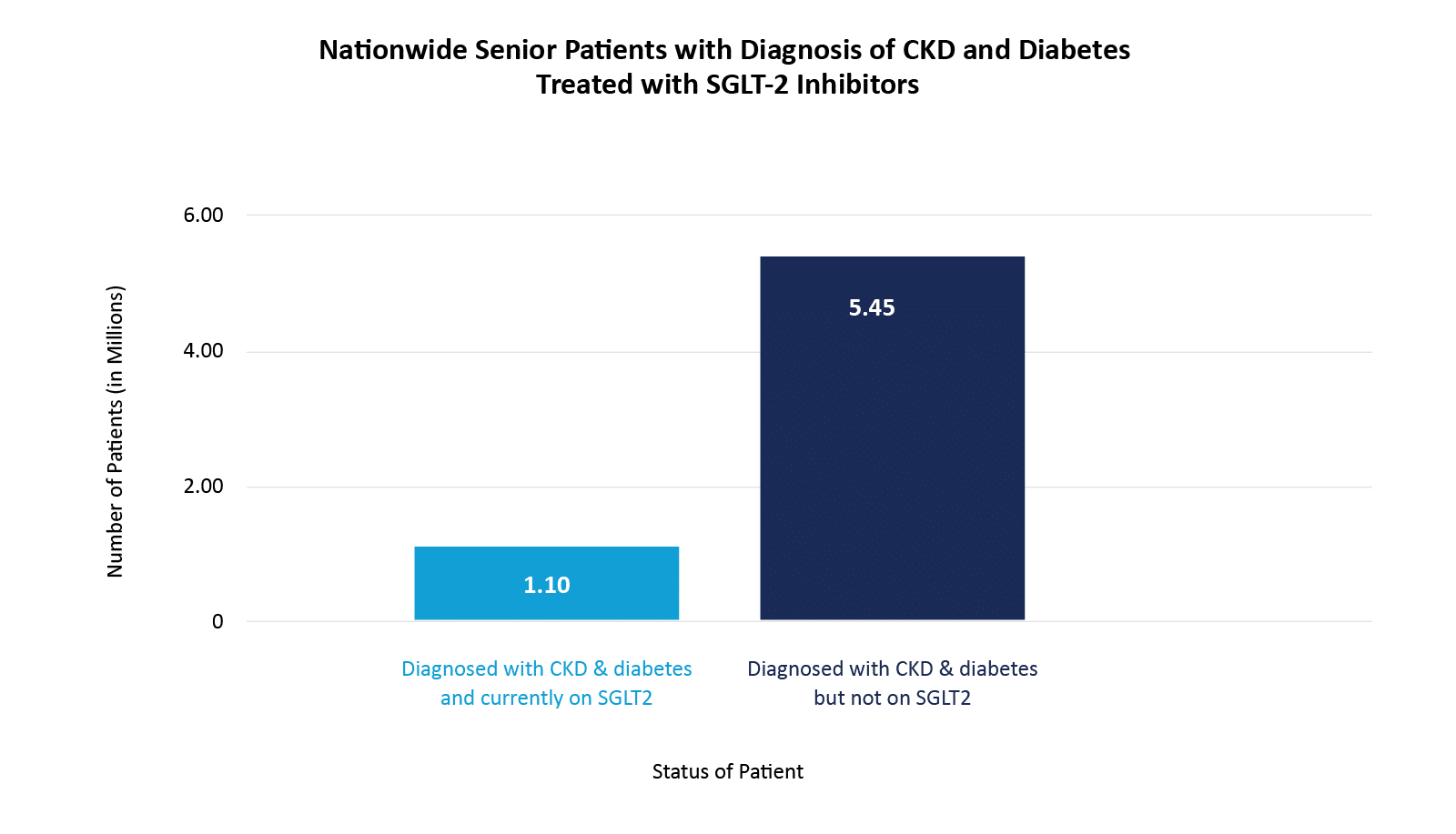
Note: Senior population defined as over the age of 65.
Data: Carenostics analytics of CareJourney transitional Medicare claims data of the senior population. The rate of Medicare patients on treatment is 18.3%, 15.4% and 6.4% for CKD Stage 1 & 2, Stage 3, and Stage 4 & 5, respectively.8
Key Takeaways
- Chronic Kidney Disease (CKD) is a silent epidemic that affects 37M Americans; 80% of people with the disease are undiagnosed and untreated.
- New, targeted therapies have become available to significantly improve patient outcomes, such as SGL2 and nonsteroidal MRAs which could delay patients’ end-stage kidney disease (ESKD) by 15 – 25 years, but patients are being undertreated.
- Only 16.8% of senior patients diagnosed with both CKD and diabetes are currently on SGLT2 treatment, which is proven to improve outcomes for this sub-population, and fewer still are on newer therapies, such as non-steroidal MRA inhibitors.
- Closing treatment gaps in patient diagnosis and guideline-directed medical therapy can improve patient outcomes, reduce unnecessary suffering, and significantly reduce costs.
Stay tuned for our next article: CareJourney and Carenostics are using CareJourney data to help map areas with greater health inequities in CKD care.
- “Chronic Kidney Disease in the United States, 2021.” Centers for Disease Control and Prevention, 12 July 2022, www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html.
- CE;, Ku E;Johansen KL;McCulloch. “Time-Centered Approach to Understanding Risk Factors for the Progression of CKD.” Clinical Journal of the American Society of Nephrology : CJASN 2018 May 7;13(5):693-701. doi: 10.2215/CJN.10360917. PMID: 29602779; PMCID: PMC5969480. pubmed.ncbi.nlm.nih.gov/29602779/. Accessed 17 June 2023.
- “Chronic Kidney Disease Basics.” Centers for Disease Control and Prevention, 28 Feb. 2022, www.cdc.gov/kidneydisease/basics.html.
“Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease.” Kidney inter., Suppl. 2013; 3: 1–150. kdigo.org/guidelines/ckd-evaluation-and-management/ - “Chronic Kidney Disease Change Package.” National Kidney Foundation, 12 Oct. 2020, www.kidney.org/contents/chronic-kidney-disease-change-package.
- “Annual Data Report.” National Institute of Diabetes and Digestive and Kidney Diseases, usrds-adr.niddk.nih.gov/2022/chronic-kidney-disease/6-healthcare-expenditures-for-persons-with-ckd. Accessed 17 June 2023.
- Meraz-Muñoz AY, Weinstein J, Wald R. “eGFR Decline after SGLT2 Inhibitor Initiation: The Tortoise and the Hare Reimagined,” Kidney360 2(6):p 1042-1047, June 2021. | DOI: 10.34067/KID.0001172021. Accessed 17 June 2023.
- “CDC Surveillance System: Percentage of Patients with CKD and Diabetes Using SGLT2i.” Centers for Disease Control and Prevention, nccd.cdc.gov/ckd/detail.aspx?Qnum=Q719. Accessed 17 June 2023.
- Kintscher U, Bakris GL, Kolkhof P. “Novel non-steroidal mineralocorticoid receptor antagonists in cardiorenal disease.” Br J Pharmacol. 2022 Jul;179(13):3220-3234. doi: 10.1111/bph.15747. Epub 2022 Jan 13. PMID: 34811750.
