As the United States continues to move toward value-based care, a great deal of attention has been given to vulnerable patient populations. Patients with higher needs (and correspondingly higher costs) are among those who would benefit most from healthcare improvement efforts, but those costs can represent significant risk to networks that stake their revenue on cost savings. One such group is the cohort of dual eligible beneficiaries (Duals), those with both Medicare and Medicaid coverage. From the special challenges they present to the elevated need for targeted interventions, Duals hold a unique place in the evolving healthcare landscape.
How Do We Account for Risk in Dual Populations?
Medicaid and Medicare were both created to ensure healthcare to vulnerable populations: the lower income and the elderly or disabled, respectively. Duals represent a particularly high-need population, falling into both categories.
In a cost-sharing model, these needs can translate to risk to providers, as Duals can require more intensive care. To mitigate this, the patient’s risk level (calculated using a combination of demographic and diagnosis data) is used to predict what their cost of care ought to be, relative to the average patient. This is intended to offset the patient’s risk by factoring it into the benchmarks against which providers are compared. Those with sicker or higher risk patients are expected to spend more on their care, so they are not penalized for serving a needier cohort. In fact, Duals are specifically prioritized in several models, such as the ACO REACH model, where they receive an additional modifier to their risk score in addition to the usual metrics.
So, what do these needs look like in this risk model? If we look at all Medicare Fee for Service (FFS) patients in 2020, the average non-Dual patient had an HCC score (prior to normalization) of .85 (meaning their care was expected to cost 85% of the average), while Duals had an average score of 1.26 (so their care was expected to cost 126% of average). This means that a Dual patient was expected to cost approximately 48% more than a non-Dual patient.
Fill out the form above to access state and county-level comparisons of Dual vs. Non-Dual avoidable ED visits, annual wellness visit and flu compliance, and more.
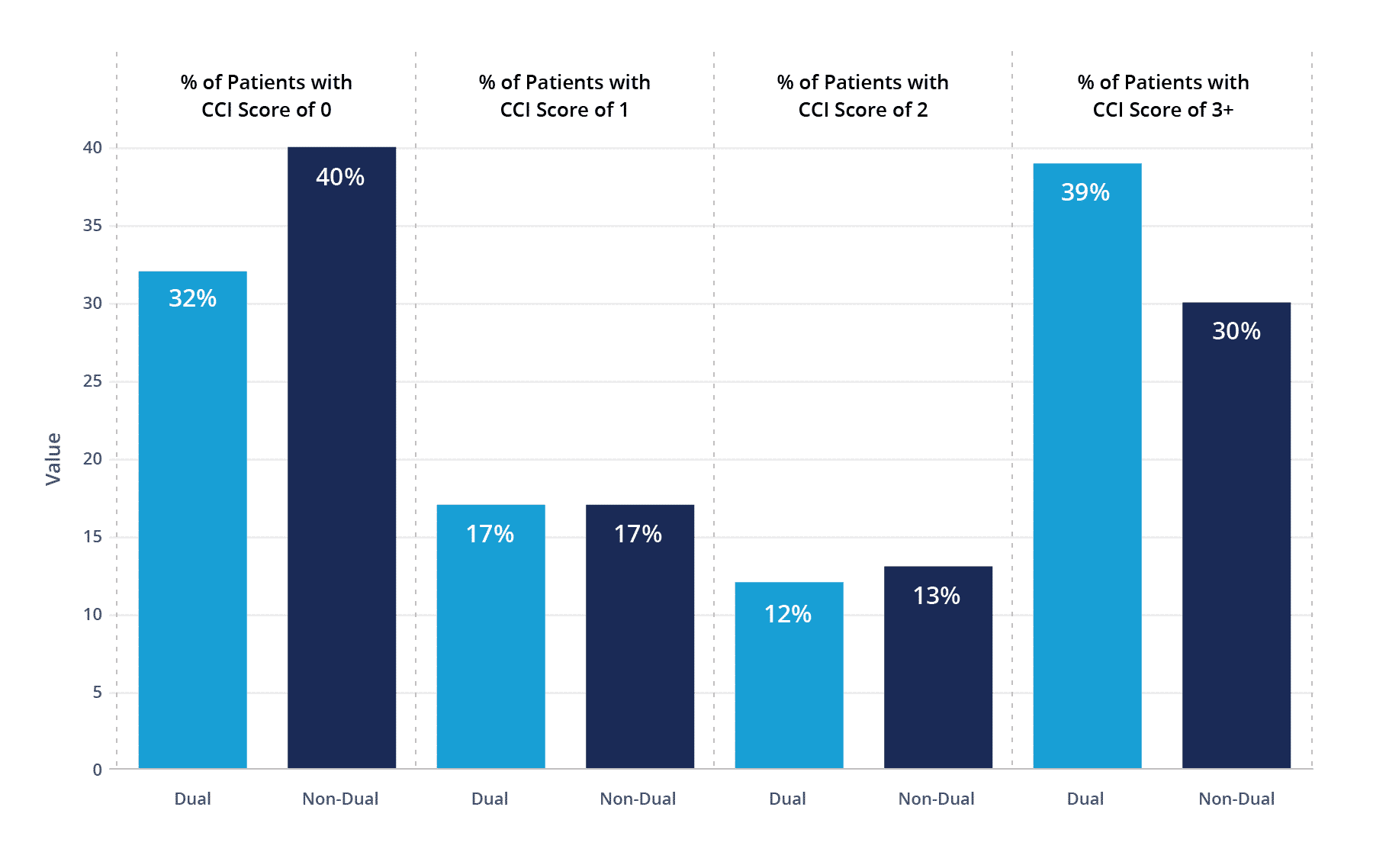
If we look at the diagnosis component to risk, Duals are significantly overrepresented in having multiple chronic conditions. 39% of Duals had a CCI score of 3 or more, compared to 30% on non-Duals. So, it is not just their demographic data, but also their diagnoses that make Duals a higher-needs cohort.
Distribution of CCI Scores for Duals vs Non-Duals in 2020
How Do These Risks Translate to Costs?
Ideally, the costs of care for Duals would be proportionate to their risk score, as that is intended to account for their elevated needs. However, that is not always the case. In 2020, the average non-Dual patient had an annual cost of $9,186 whereas the average Dual patient had an average cost of $16,372 – a striking 78% difference compared to their non-Dual counterparts.
There are several reasons why the current costs outstrip the risk models. As noted in our previous blog, under the Medicare FFS model, chronic conditions are often undercoded, meaning high needs patients may have artificially low risk scores. Additionally, previous models have further underestimated high-needs patients by not adequately accounting for patients’ Social Determinants of Health (SDoH), a problem which newer models are working to remedy.
Another factor in health costs is the type of care patients are receiving. Duals, who account for 19% of the Medicare FFS population, represent 38% of avoidable ED visits, a costly and unnecessary expense. On the other hand, Duals are only 15% compliant on receiving annual wellness visits (compared to 29% of non-Duals) and 32% compliant on receiving their flu vaccine (compared to 57% of non-Duals). So, while significantly more is being spent on their care, it is not necessarily being spent on the preventative care necessary to reduce overall costs and improve patient outcomes.
Access Data Comparing Dual and Non-Dual Populations
At state and county levels, see population differences in metrics like average risk score, total PMPY, flu compliance, and more.
Opportunities for Better Serving Duals
While the increased costs of Duals may seem to be a deterrent, there are a number of opportunities to make a meaningful impact on one of the most high-need cohorts. In the new ACO REACH model, ACOs are allowed to increase their year-over-year risk score growth cap when the demographic component1 of the score increases. This allows practice groups to expand their cohort of Duals without worrying about capping out on their risk adjustments.
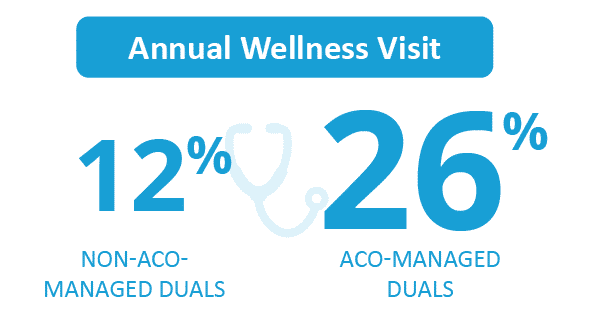
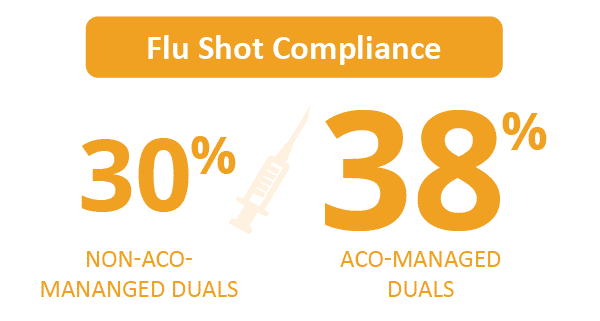
If we look at the 2020 Dual patients, we can already begin to see the impact ACOs are having with reducing costs and meeting patient needs. Duals who were managed by ACOs had an average risk score of 1.44, compared to 1.25 for Duals who were not. As networks are incentivized to properly code chronic conditions, the risk scores for these patients more accurately reflect their level of need, which is then reflected in the network benchmarks. ACO-managed Duals were 26% and 38% compliant for annual wellness visits and flu vaccines, compared to 12% and 30% for Duals not managed by ACOs.
In terms of costs, Duals managed by ACOs had an average annual cost of $16,321, compared to $16,389 for Duals not in ACOs. Even with much higher compliance rates in preventative health among ACO-managed Duals, there is very little difference in their overall costs. This suggests that deeper investigation is required into how to better serve this patient cohort.
Participating in the ACO REACH Model?
Learn how to be successful in the model.
Part of the Medicare Shared Savings Program (MSSP)?
Learn how to improve performance in MSSP.
How CareJourney Can Help
CareJourney is an industry leader in providing the analytics and insights necessary to manage your network, including:
- Cohort profiling to understand your dually eligible populations and opportunities to improve their outcomes.
- Network management to identify providers managing care for populations of interest.
- Support in understanding payment models and network development considerations to best reach and serve dually eligible patients.
For more information on how CareJourney can partner with you, please request a demo.
Not ready for a meeting? Check out our resources to learn how CareJourney helps payer, provider, and pharma organizations reduce the total cost of care and improve care quality.
- The Demographic component of the risk score consists of age, gender, whether a patient is dually eligible, and whether the patient originally became eligible for Medicare due to a disability.
