How to Identify Patient Intervention Opportunities up to 5 Weeks Sooner with BCDA
By Rachel Plummer and Chris Freyder
March 25, 2024
What is BCDA?
In today’s rapidly evolving healthcare landscape, access to real-time data can profoundly impact clinical outcomes. The Beneficiary Claims Data API, or BCDA, is a cutting-edge tool that brings timely healthcare claims and beneficiary data to the forefront. Centers for Medicare and Medicaid (CMS) offers BCDA access to certain value-based care entities including Accountable Care Organizations (ACOs) engaged in the Medicare Shared Savings Program (MSSP), ACO Realizing Equity, Access, and Community Health (ACO REACH), and Kidney Care Choices (KCC). BCDA offers adjudicated claims to these model participants, but additionally offers partially adjudicated claims to ACO REACH entities, which allows for even quicker access to claims that enter Medicare’s system that have not yet been fully paid or processed by CMS. These data enhance operational activities for model participants, giving them a better shot at success in their performance year. In this piece, CareJourney dives deep into the nuances of BCDA claims, compares them with other common data feeds, and discusses the potential value across a handful of use cases.
Why It Matters: The Use Cases of BCDA
Real-time insights via BCDA can facilitate proactive interventions, reducing potential financial burdens like costly visits to the emergency department (ED) or avoidable inpatient admissions. Timely BCDA data feeds paired with predictive modeling, which may identify individuals at risk of hospital readmission or developing specific health conditions based on claims history, care managers can check in with high-acuity patients to optimize treatment plans and mitigate the risk of adverse events. Any delay or inefficiency in data access can lead to delays in intervention, which may result in less-than-ideal patient care and escalate downstream costs.
Beyond cost considerations, BCDA is valuable when used in combination with admission, discharge, and transfer (ADT) feeds. While ADT’s timeliness is similar if not better than BCDA, it faces two significant limitations: first, the technology lacks comprehensive coverage and is not supported by all facilities, leading to gaps in information for specific patient groups or geographic areas. Second, its focus remains largely on hospitals, sidelining other vital services like home health, ambulatory and other professional care. These professional services, including visits with specialists, laboratory tests, and prevention screenings, provide valuable insights into beneficiaries who don’t require hospitalization, but still require regular medical attention. Thus, crucial elements of care coordination and coding gaps are missed when relying on ADT data alone.
Finally, these ACO programs have traditionally relied on the Claim and Claim Line Feed (CCLF) files containing Medicare Parts A, B and D claims and enrollment data to assist with care coordination efforts, accessed on a monthly basis via CMS data hubs. However, BCDA offers a significant edge, particularly in claim timeliness, given CCLFs provide delayed insights ranging from 45 to 60 days from the point of care. Though we will delve deeper into this in the subsequent section, it’s worth noting here that BCDA’s promptness in delivering data insights outpaces that of CCLF. This rapid access to data not only accelerates decision-making but also broadens the horizon for what’s possible in patient care.
Descriptive Statistics on BCDA Timeliness
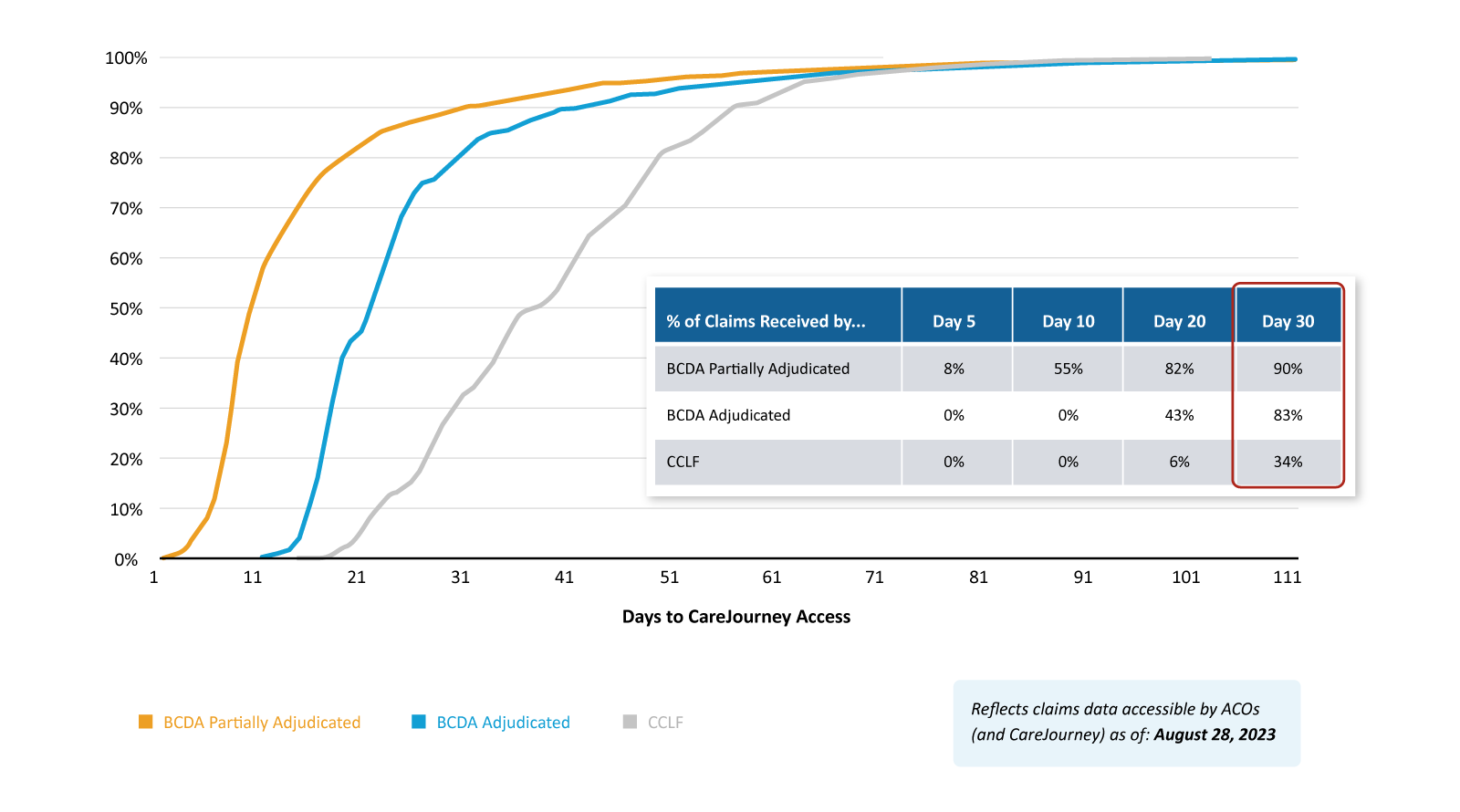
A comparative lens on BCDA and CCLF data timeliness reveals some stark disparities. Figure 1 offers a compelling narrative. Just 30 days after a service occurs, BCDA showcases a partially adjudicated claims retrieval rate of 90% and a fully adjudicated claims retrieval rate of 83%, leaving CCLF trailing at 34%. This ensures providers are equipped with insights faster, translating to swifter interventions. In the past, CCLFs were generally not as useful until you received three months of claims runout. BCDA, however, can offer a distinct advantage in providing more data and early indicators of spending trends just one month out.
Figure 1
Further, while CCLF lags take six to seven weeks for important notification of events like ED visits, inpatient admissions, and annual wellness visits (AWVs), BCDA hits this mark in just two to three weeks. This four to five-week difference can be instrumental, especially in scenarios that demand timely interventions. Figure 2 showcases that for a sample ACO REACH entity with nearly 8,000 aligned beneficiaries, the BCDA source would have identified nearly 300 additional AWVs, 400 more ED visits and 160 more inpatient discharges by the middle of the performance year that they would not have otherwise known about through the CCLF source.
Figure 2

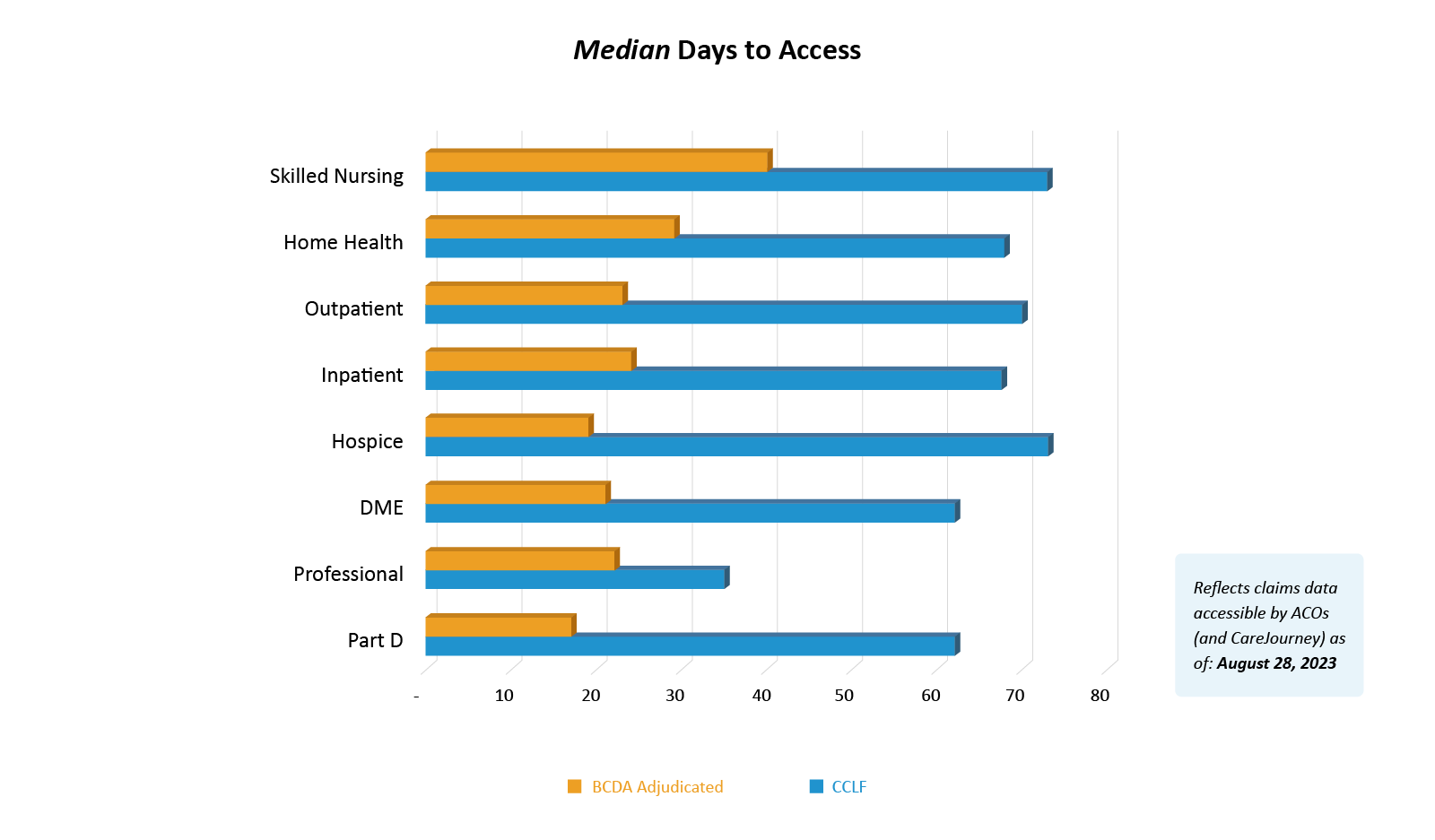
The overarching theme of efficiency is driven home by Figure 3. Across all claim types, BCDA processes claims about 50% faster than its CCLF counterpart, a testament to its superior data retrieval capabilities.
Figure 3
The Potential for Early Intervention
BCDA provides healthcare professionals invaluable insights into patient health trends, showing significant promise in identifying high-risk patients earlier. The timeliness empowers clinicians to intervene earlier, which can reduce the risk of complications and improve patient outcomes overall.
Comparing claims data sources reveals how care teams that leverage BCDA would’ve captured patients with cancer or who have suffered a stroke at an earlier stage. When analyzing adjudicated claims data, specifically ICD-10 diagnosis codes billed within a 2-year lookback period, more relevant prevalence rates of chronic conditions can be determined through BCDA as compared to CCLF. For example, based on data loaded during the performance year for a sample ACO REACH entity with over 50,000 aligned beneficiaries, we uncovered an additional 30 beneficiaries with breast cancer and 60 more beneficiaries who have suffered from a stroke when utilizing BCDA data, as opposed to CCLF. Figure 4 also highlights a consistent increase in patient counts for each of these chronic conditions across three weeks of BCDA incremental data loads, indicating the rising trend and potential need for proactive management of these patients.
Figure 4
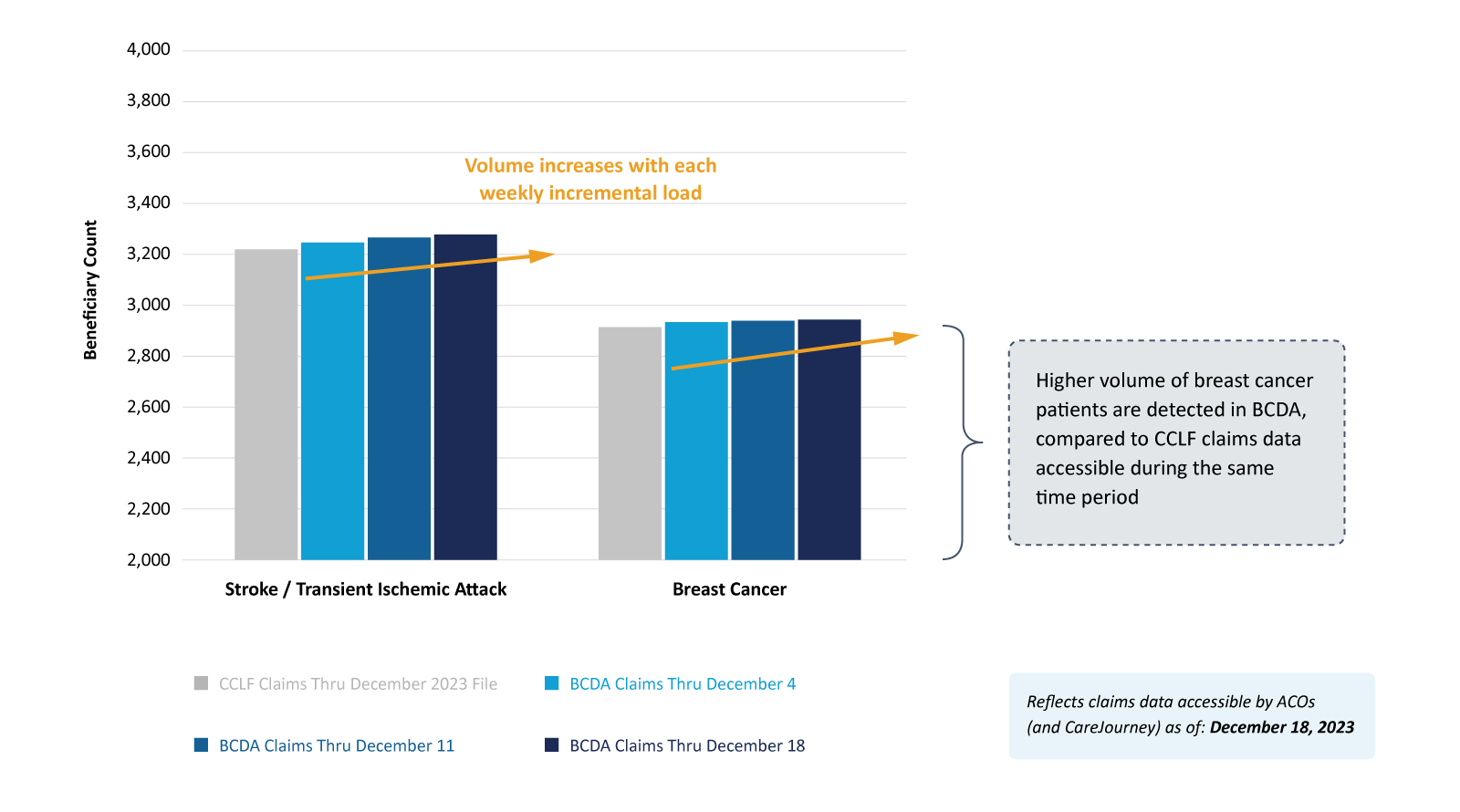
Timely medical claims data can empower healthcare decisions that enable prompt interventions that both enhance patient outcomes and yield long-term cost savings. One study suggests that even delays of just a few weeks in initiating treatment for metastatic breast cancer can significantly impact survival outcomes, with delays exceeding 12 weeks showing particularly adverse effects.
Conclusion
When accessed and interpreted promptly, data can catalyze transformative healthcare practices. BCDA redefines how ACOs access and utilize their data. Its swift data retrieval mechanisms, coupled with the comprehensive CareJourney insights layered on top of the data, ensure care providers are always armed with the most current information. As we move towards a future of efficient and coordinated care, BCDA aims to support ACOs in their goals of enhancing clinical efficacy, reducing cost, and improving care quality.
How CareJourney Can Help
Harnessing the full potential of BCDA requires technical expertise and a robust ingestion pipeline that handles security, quality assurance, and daily loading of semi-structured data in JSON format delivered via Fast Healthcare Interoperability Resources (FHIR®) standards.
A 10-year veteran in value-based care, CareJourney remains at the forefront of building advanced analytics that are accessible in innovative ways. CareJourney ingests your ACO’s BCDA data to generate practical insights and enhanced analytics built on top of these claims. Our solutions empower your ACO to deliver the highest quality care. By continuously updating this data and refining insights, CareJourney ensures you always have a finger on the pulse of your population’s health. Read more about accelerating care coordination with BCDA analytics.
If you’re a CareJourney member interested in a free trial of these expedited insights, email support@carejourney.com. If you are not a member, email info@carejourney.com.

