Drivers of Value-based Care Success
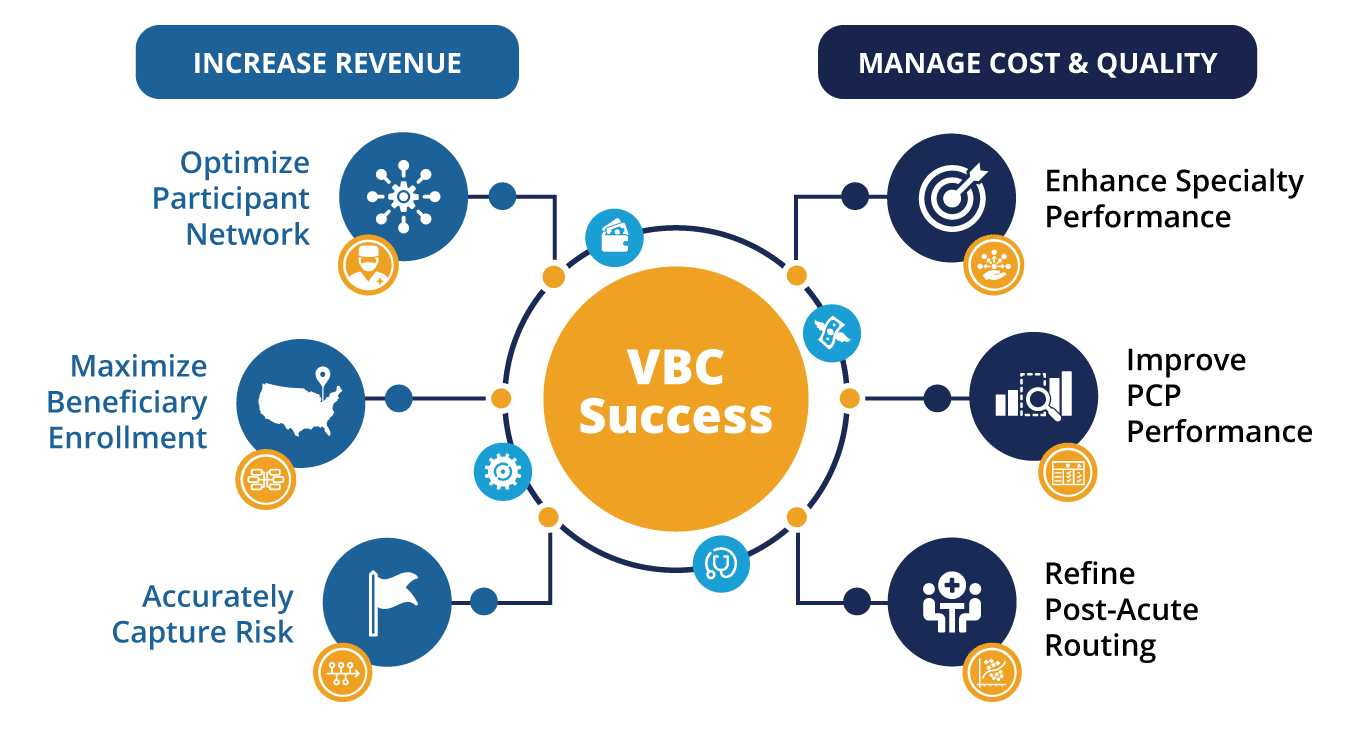
As healthcare spending becomes unsustainable and fee-for-service models give way to advanced payment models, value-based care organizations (VBOs) must confidently and continually optimize their operations to best care for patients and stay in business.
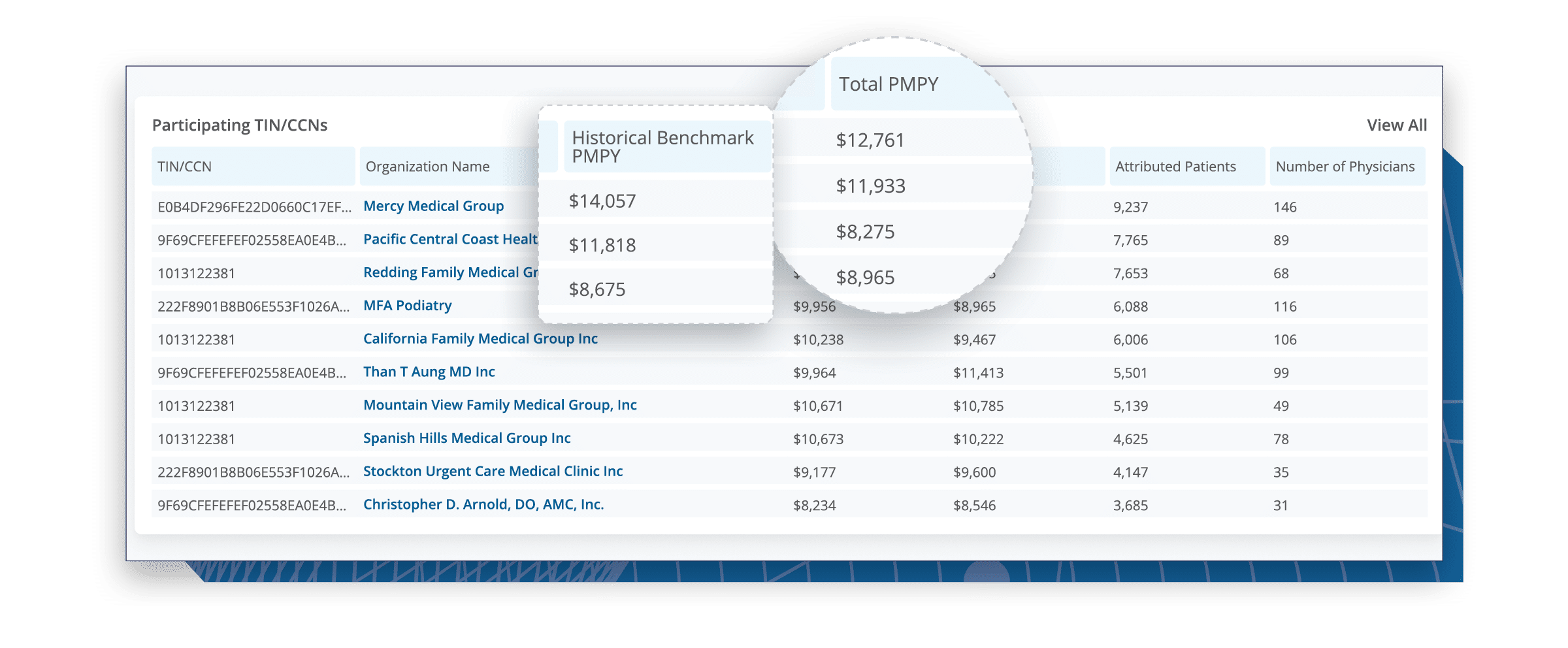
A 9-year veteran in the value-based care industry, CareJourney® helps 150+ innovative VBOs grow their entities, improve care quality, and reduce costs using the most robust, detailed, comprehensive claims dataset available.
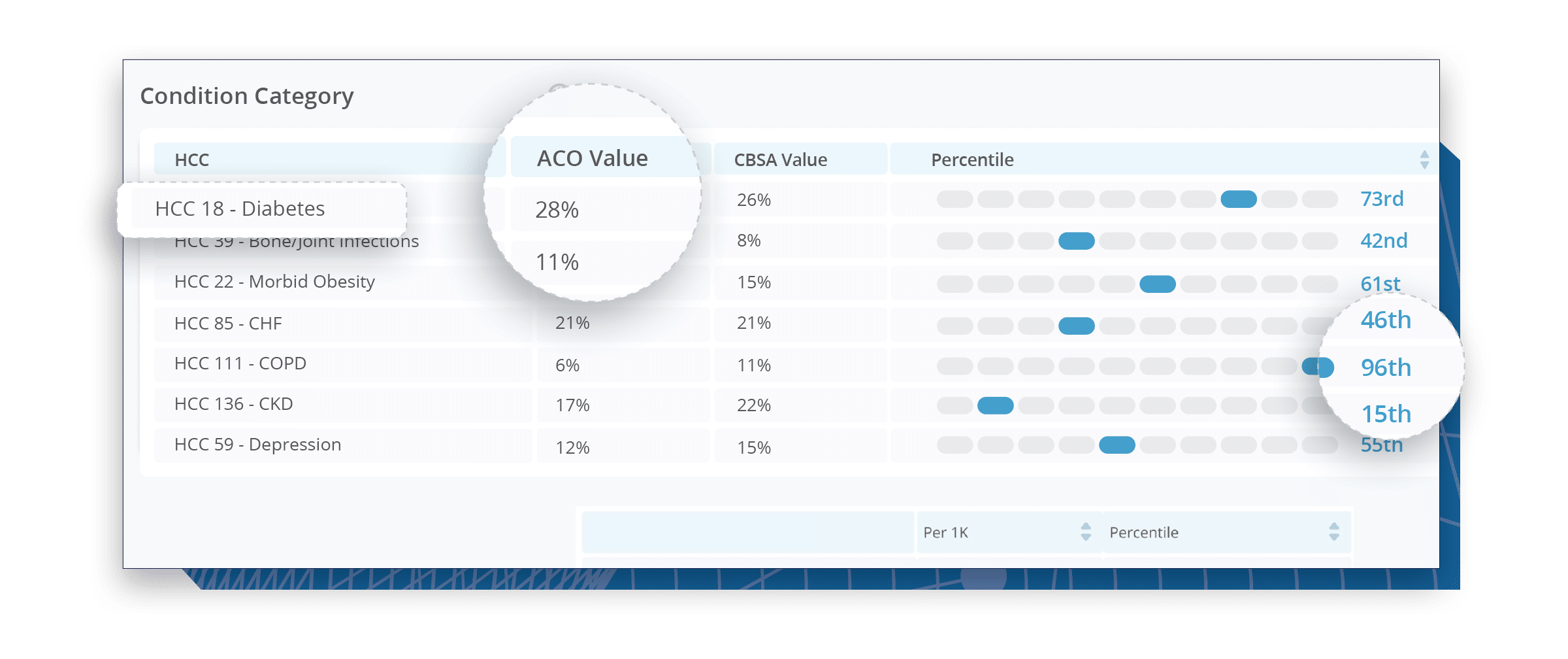
CareJourney analytics are derived from Medicare, Medicaid, Medicare Advantage and Commercial claims data, unlocking insights on over 300 million beneficiaries and 2 million providers. With open and transparent methodologies, CareJourney’s 250+ episodes benchmarked make both care decisions and business decisions a no-brainer.
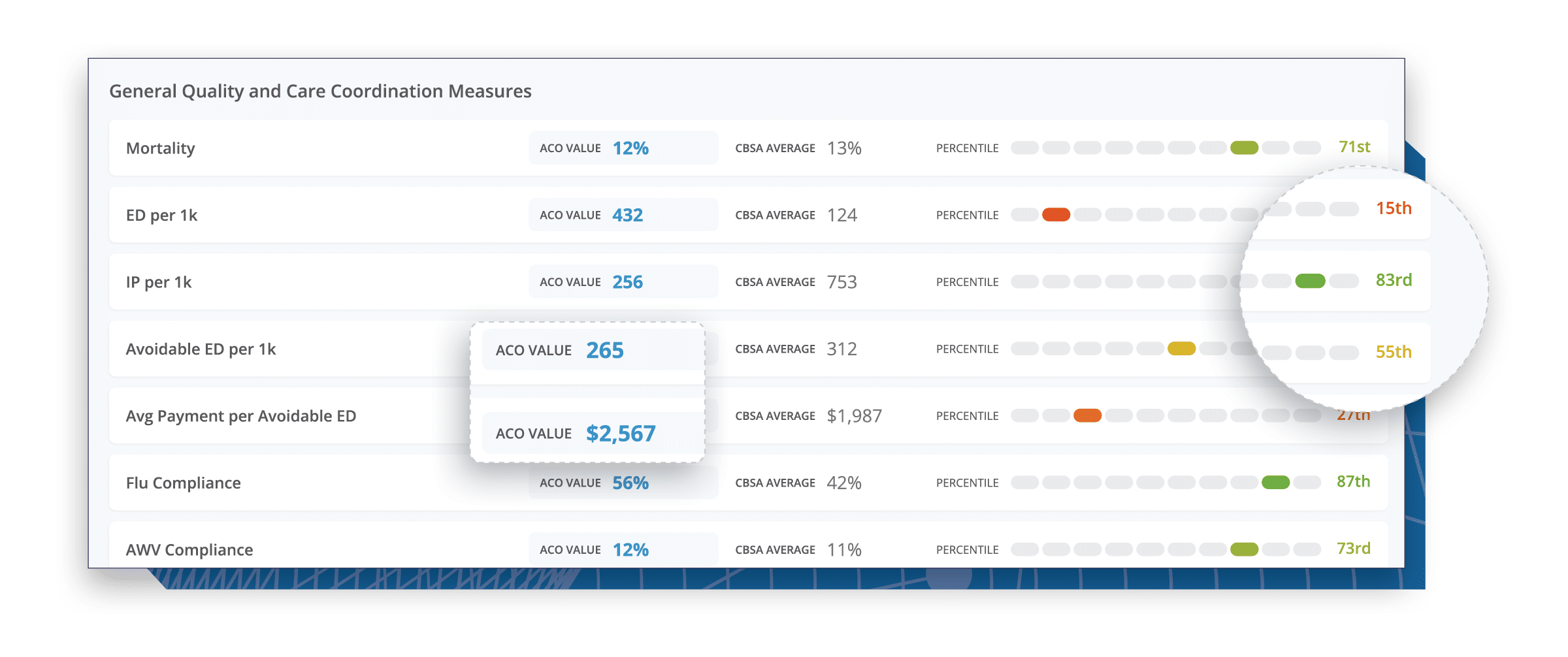
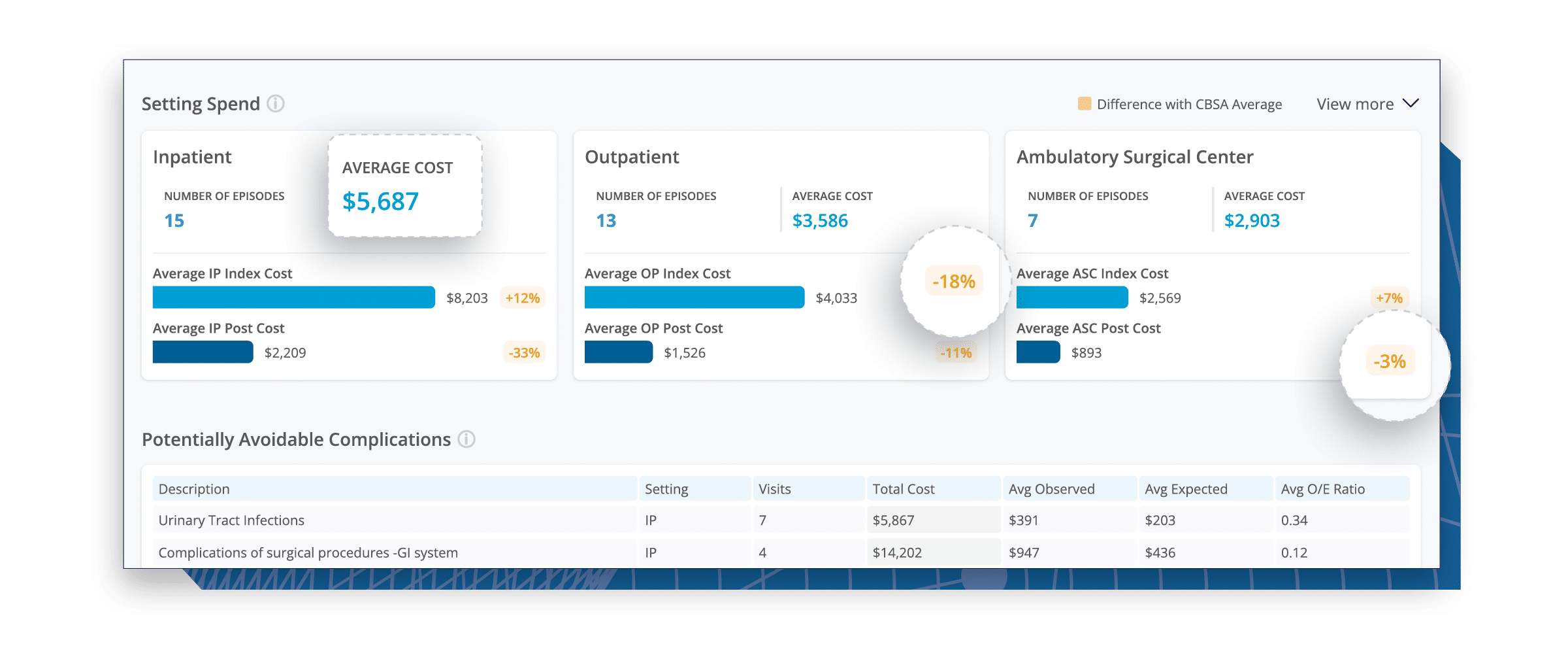
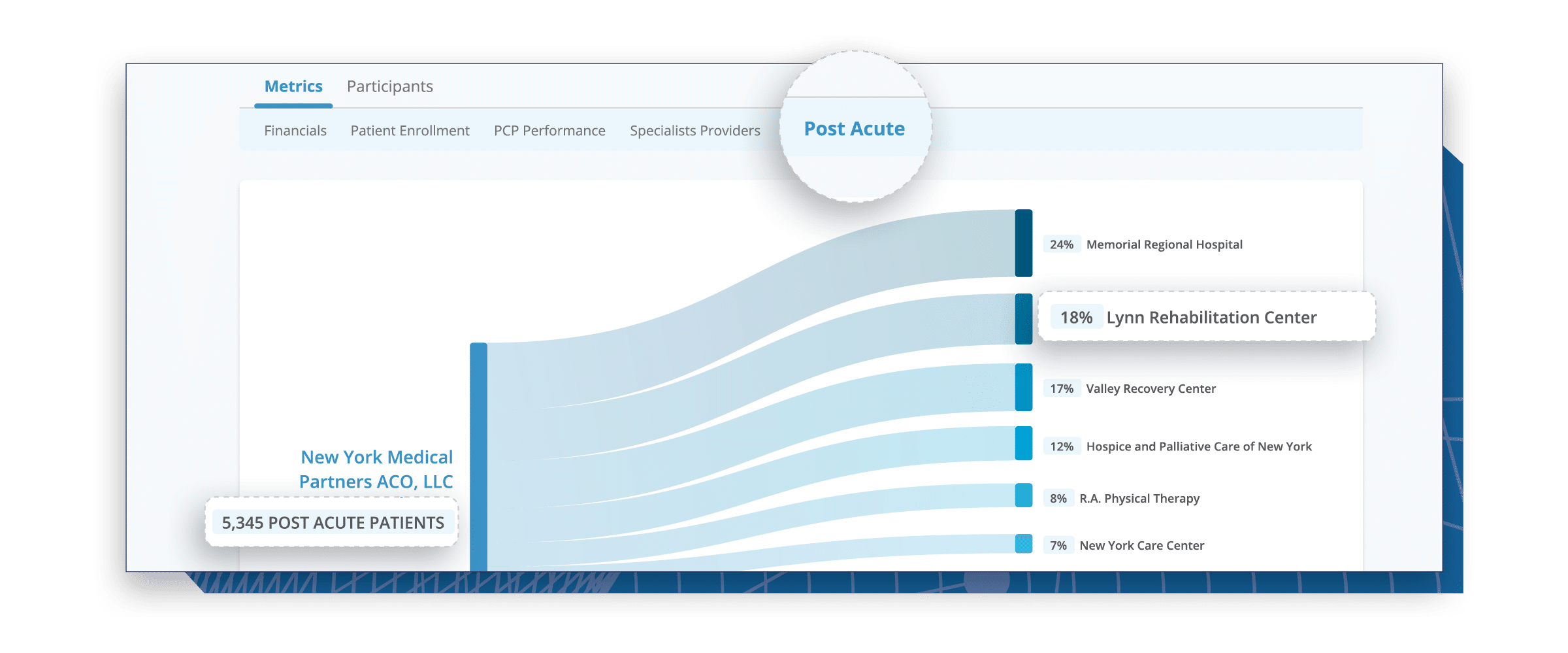
Organizations achieving success in this evolving landscape trust CareJourney insights to guide their strategy and operations across six specific areas that directly correlate with either increased revenue, cost reduction, or quality improvement.
Member Testimonials