For Payers That Want to Make Data-Driven Decisions
To succeed in today’s data-driven world, Payers need advanced analytics with actionable insights to reduce costs and improve outcomes for their members.
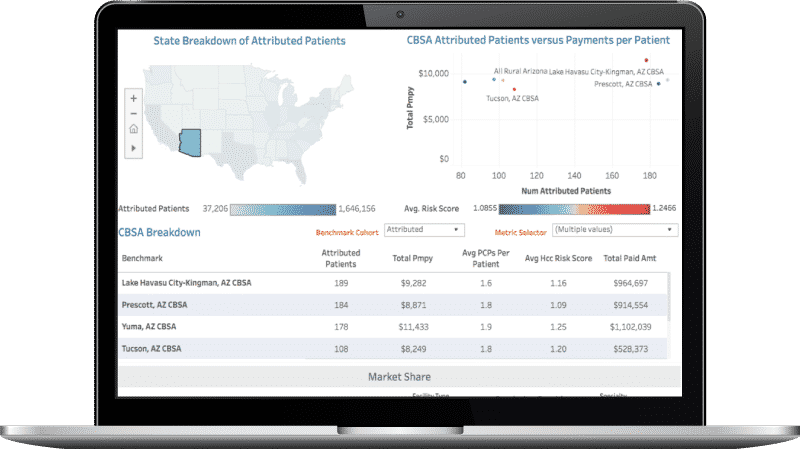
Our healthcare payer analytics help you gain market intelligence, find the right providers and specialists to partner with, and understand risk for your patient populations. Our health plan solutions provide insights derived from our access to comprehensive Medicare, Medicaid, and Commercial datasets – linked claims and encounter data for over 300 million longitudinal beneficiaries. You can use our healthcare payer analytics to build and optimize your network, evaluate your performance against the rest of the market, and take action to increase your footprint.

Our analytics platform offers clinically-relevant insights to understand market share, identify high-need patients, build high-performing networks, and improve provider performance and patient outcomes. It is powered by one of the largest claims datasets in the country that is backed by comprehensive and transparent methodologies.
Find all the relevant information needed to be successful in value-based care, all in one place.


“CareJourney’s analytics have allowed us to identify high-performing providers and map them to the right patients that need the most care. We were able to successfully expand our network into new geographies and evaluate network performance and adequacy over time.”
Chief Strategy and Growth Officer
Large Regional Payer
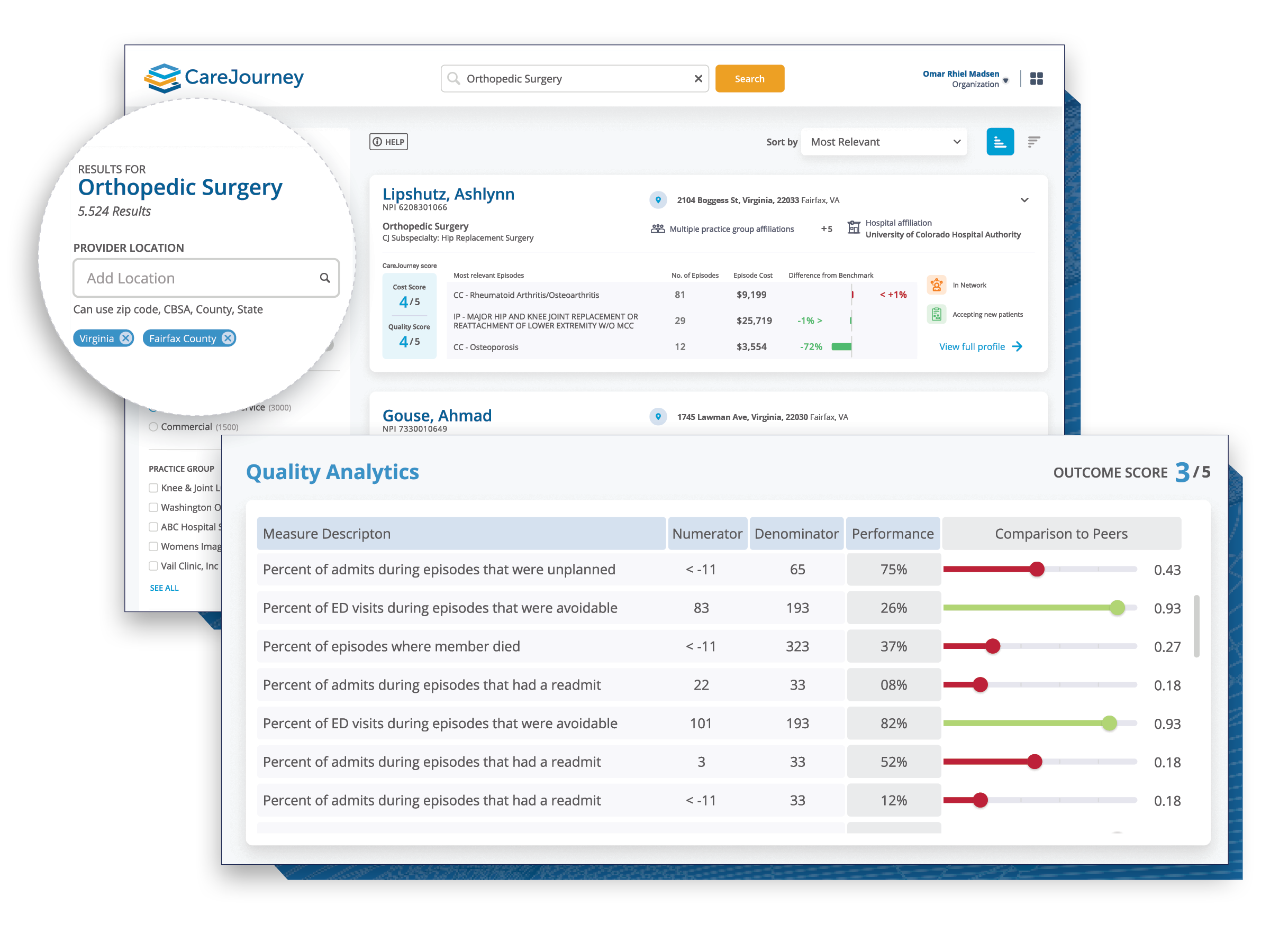
This guide presents an overview of tools for implementing network selection, management, and optimization using CareJourney’s Provider Performance Index for cost and outcomes.
A growing Health Plan used CareJourney to pinpoint the best market participants, expand to new markets across the nation, and achieve high network integrity between providers, groups, and facilities.
CareJourney provided utilization patterns and referral views to understand which Specialists were already being utilized heavily by existing in-network primary care providers.