Provider Data: The Critical Elements to Getting it Right
By Joe Mercado, MBA, MS
November 7, 2023
In our last blog, Provider Data: How it Can Make or Break Your Value-based Care Strategy, you learned what makes provider data important. Now that you have the basics down and understand the stakes of poor quality data, it’s time to dig into the critical role that analytics play. In this blog, we will talk about the importance of analytics in measuring and evaluating providers, and the high stakes of getting it right.
The Critical Requirements to Getting Provider Performance Right
Before we begin, let’s start by understanding the specific elements required to be able to successfully build a provider performance analytics asset.
- Risk Adjustment: Risk adjustment methods are crucial for comparing two providers, ensuring that you’re factoring things like patient panel (and characteristics), location, and more. You can also create expected values which allow you to classify if providers are outperforming what is expected of them. While no risk adjustment model can account for all clinical variation between patient populations, a robust model is necessary: historic HCC generally only accounts for 20% of the patient spend.
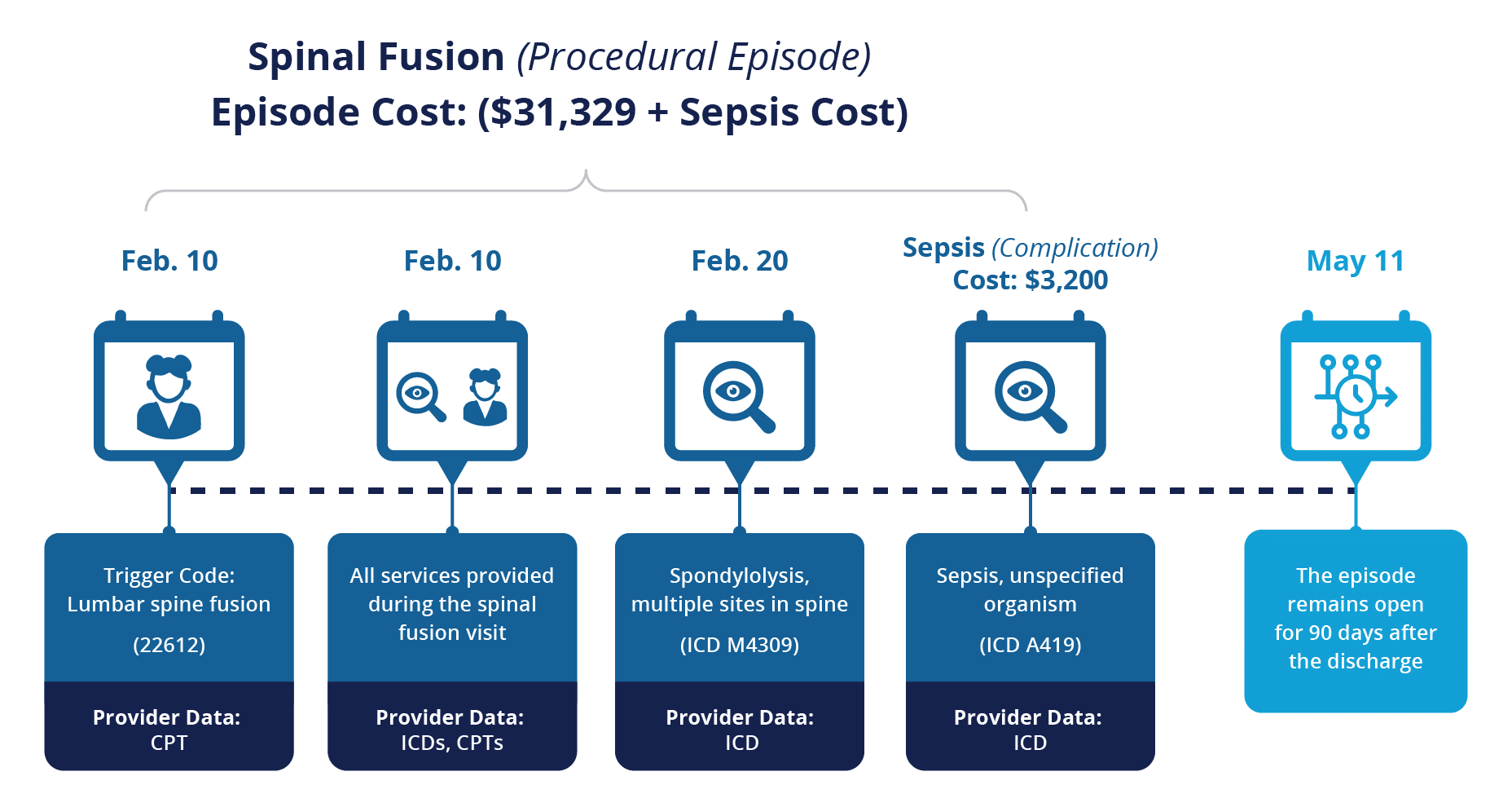
- Episodes: Grouping individual services into episodes is necessary to depict a full picture, and enable comparisons for care variation. Episodes allow you to look at care variation for spinal fusion versus the individual service like a Laminectomy.
- Attribution: Clinically-relevant attribution, available at multiple provider levels, is needed to do this right. Depending on your use case, the triggering provider (i.e., surgeon) may make the most sense, whereas in other situations, the attributed provider may make more sense.
- Quality: Understanding how a provider treats a panel with respect to outcomes, process, and appropriateness is important as you build networks, understand performance variation across providers, and determine the right provider for your referral at the point of care.
- Multiple Lines of Business: While some may assume that practice patterns remain consistent across lines of business, evaluating performance on a single line of business can be fraught with issues, introducing a number of biases.
- Geographic Comparisons: Given the geographic nuances of particular markets, it’s important to only compare those practicing in similar regions. This is particularly crucial for referrals. You don’t want to send a patient for a referral in NYC if they live in Kissimmee, FL (unless there is another reason that they aren’t privy to).
- Comparing Like Providers: When comparing providers to one another, it’s critical to ensure that you are comparing those who perform similar services, i.e., spine surgeons who do spinal fusions primarily in the outpatient setting.
- Measuring Multiple Providers: Often, groups define a provider as the set of NPIs treating a patient. However, this is a limiting view, as there are many different entities with important variations across the patient journey.
- Drill Downs: Without the ability to drill down into the “why” behind any of the analytics, you’ll only have surface level conversations. This critical element is often overlooked because it’s difficult. For instance, if a group wants to understand if a surgeon’s cost and outcomes are being impacted by high use of skilled nursing facilities, the ability to drill down is necessary.
| Requirements | Informed Decision Making (i.e., Referrals) | Performance Benchmarking | Variations of Care | Provider Profiling | Quality Improvement Initiatives |
|---|---|---|---|---|---|
| Risk Adjustment | x | x | x | x | x |
| Episodes | x | x | x | x | |
| Attribution | x | x | x | x | |
| Quality | x | x | x | x | x |
| Multiple LOB | x | x | x | x | x |
| Geography Comparisons | x | x | x | x | |
| Comparing Like Providers | x | x | x | x | x |
| Multiple Provide Types | x | x | x | x | x |
| Drill Downs | x | x | x | x | x |
CareJourney’s Provider Performance Index includes all of these requirements in the construction so as to enable members to explore their potential.
The Role of Analytics in Provider Performance
Provider performance data alone is valuable, but its true potential is unlocked through analytics. Analytics add a layer of intelligence to raw data, transforming it into actionable insights.
Those insights enable the following:
- Informed Decision-Making: Analytics enable healthcare leaders to make informed, data-driven decisions. It helps identify trends, patterns, and opportunities for improvement that may be hidden within the data. Learn how CareJourney enables its members to unlock high performance network building.
- Performance Benchmarking: Organizations can benchmark their provider performance against national or regional standards, gaining a competitive edge by identifying best practices and areas for enhancement.
- Identifying Variations in Care: Analytics can uncover variations in care patterns among providers within the same organization or network. Identifying these variations can lead to standardized care processes, reduced inefficiencies and improved quality.
- Provider Profiling: Analytics enable profiles of individual providers, showcasing their strengths and areas for improvement. These profiles can guide performance discussions, continuing education, and quality improvement initiatives. Learn how one CareJourney member leverages provider data to improve referrals.
- Quality Improvement Initiatives: Analytics guide quality improvement initiatives by identifying root causes of performance gaps and tracking the impact of interventions over time. Here’s how one organization determines which quality improvement initiatives to evaluate providers on.
In summary, analytics in provider performance are instrumental, allowing organizations to advance their decision making and become data-driven in their approach. Provider profiling, benchmarking, and variations in care are key components to consider when building your high performing network. But what happens when you do it wrong, or don’t do it at all?
The High Stakes of Ignoring Provider Performance Data and Analytics
As healthcare continues its relentless march toward value-based care, organizations that ignore provider performance data and analytics do so at their own peril. Here are the high stakes of neglecting this critical component:
- Patient Outcomes: Ultimately, patient outcomes are at stake. Without data-driven improvements, patients may receive suboptimal care, leading to poorer health outcomes.
- Competitive Disadvantage: In an increasingly data-driven industry, organizations without robust data analytics capabilities risk losing out to competitors who can better leverage data for their benefit. As organizations are building data-driven high performing networks, those without the appropriate analytics are forced to leverage out-dated or inadequate information.
- Financial Impact: Value-based payment models directly tie reimbursement to provider performance. Organizations without performance data may face financial penalties and missed incentives.
- Missed Opportunities: Failure to harness provider performance data means missed opportunities for quality improvement, cost reduction, and enhancing the patient experience.
Stay Ahead of the Curve with Provider Performance Data and Analytics
In conclusion, the importance of provider performance data and analytics are critical to success in today’s healthcare landscape. Organizations that embrace these tools position themselves for success by fostering quality improvement, enhancing patient care, and ensuring financial viability. In contrast, those without adequate analytics risk being left in the dust as healthcare continues its transformation into a data-driven, value-based industry. The choice is clear: adapt and thrive or risk falling behind.
In our next blog, we’ll discuss how volume measures can shed light into a provider’s experience treating different conditions.
How CareJourney Can Help Get You Started
With access to a large national dataset of commercial, Medicare and Medicaid claims, CareJourney has developed comprehensive provider profiles led by cost and quality metrics and their building blocks to enable care improvement and network development. Grounded in taxonomy and CareJourney’s Provider Performance Index, users also get access to demographic details to maximize additional strategies.

