Through a joint partnership under the Robert Wood Johnson Foundation’s Health Data for Action Program, Altarum and CareJourney generated a remarkable new toolset to explore trends, determinants, and interventions in cost, quality, and access issues for geriatric and gerontological care.
CareJourney and Altarum have partnered in developing a breakthrough approach in measuring care for patients with physical and cognitive disabilities, focusing on adults aged 65 and older. In our analysis of 2018 medicare FFS claims data, we identified 6.7 million traditional Medicare patients who required long-term services and supports (LTSS) and had assessments that document these conditions. Altarum developed an outcome measurement tool to visualize data at a county level with CareJourney, providing the underlying analyses that enabled exploring the value improvement opportunities among these patients.
What Does the Data Reveal?
In a time of rising populations entering old age, serving Medicare patients will require greater attention to the self-care disability and cognitive impairments that often come with elderhood. Without self-care support and care coordination, the growing segment of patients who need them will more likely face calamitous but preventable events, like falling and rehospitalizations, which contribute to high medical costs. Improving in-home support often avoids costly and harmful events in key patient groups.
Self-care disability and cognitive disability are not explicitly documented in Medicare claims, so we merged post-acute/long-term care assessments with claims using the Outcome and Assessment Information Set (OASIS) and the Minimum Dataset (MDS). We then analyzed the care patterns, quality, and costs for Medicare beneficiaries with these disabilities, thanks to funding from the Robert Wood Johnson Foundation. Self-care disability was identified in nursing assessments. We defined self-care disability as when the patient had dependence in two or more of six Activities of Daily Living, or ADLs. Cognitive disability was identified by examining mental status data in nursing assessments plus Alzheimer’s diagnoses in Medicare claims. In the following visualizations, we explore these population subsets and their measures, at the county level.
The Altarum team encourages health system leaders with strong community ties to first explore the county-level data because localized arrangements for long-term supportive services shape what care is needed and possible for these populations. The data may spur partnerships with Area Agencies on Aging or other community-based organizations that serve elder adults with disabilities. April 2020 research in Health Affairs shows that these alliances are not only becoming increasingly prevalent, but also leverage local gerontology expertise to yield savings.
CareJourney’s outcome measurement tool can provide its members the same data at different levels of analysis, such as aggregating patients according to their health care providers. We found these data to reveal rewarding opportunities to serve elder adults.
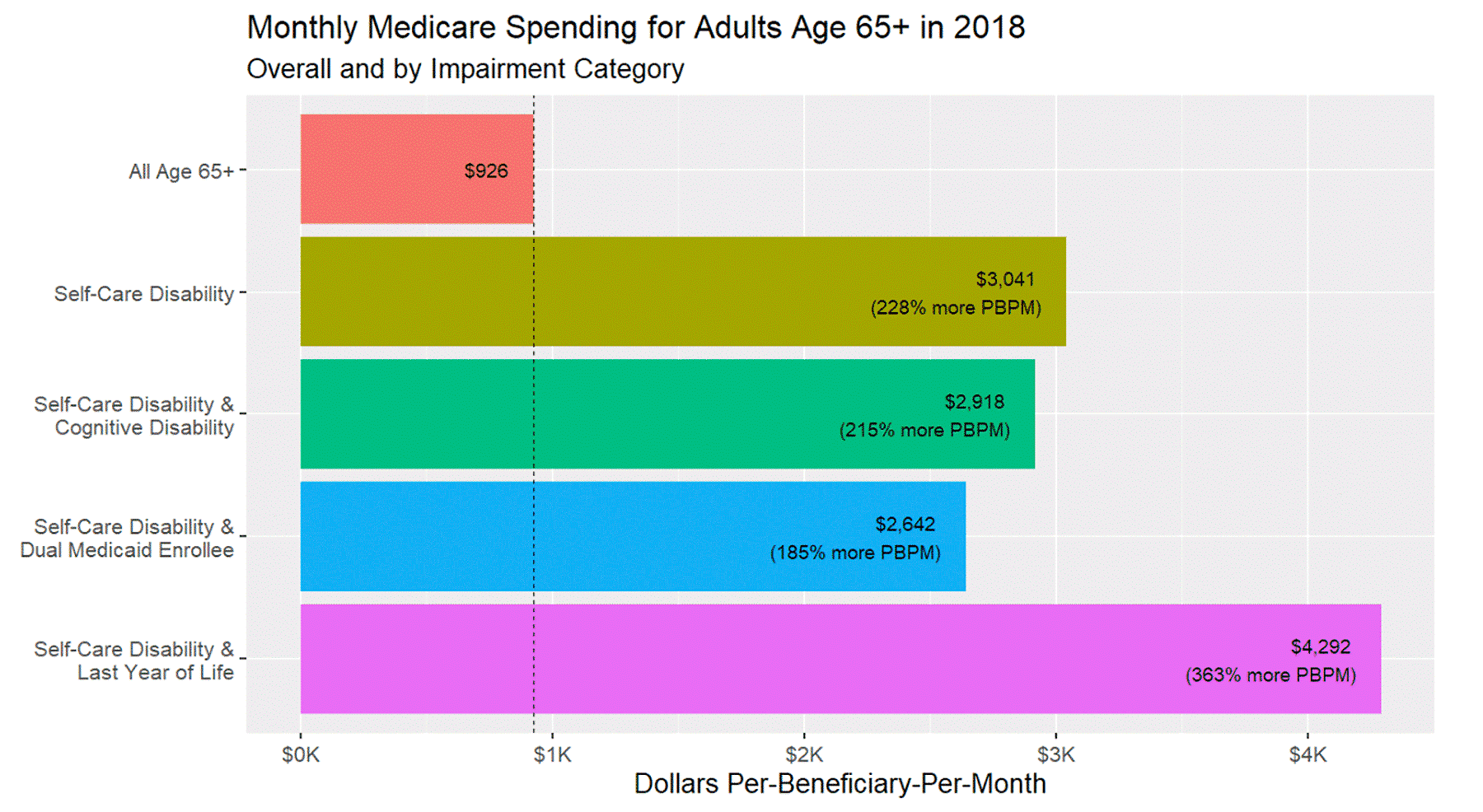
Consider the amount Medicare pays for groups of patients with self-care disability, based on 2018 data. Figure 1 indicates that for beneficiaries assessed with a self-care disability, the average PBPM spending was $3,041. That was 3 times the average PBPM for all persons over the age of 65 who we analyzed, at $926. In a separate analysis (not shown), we found that spending in the last year of life for beneficiaries with a self-care disability was more than 70% higher than all other beneficiaries’ end-of-life spending, at $4,292 for those with disability versus $2,523 for the others.
FIGURE 1: National Medicare Spending for Elder Adults and Groups with Impairments
Our analysis also shows wide variability in these spending figures across counties. We found areas with favorable quality indicators despite low spending – but also areas with high spending and unfavorable quality indicators.
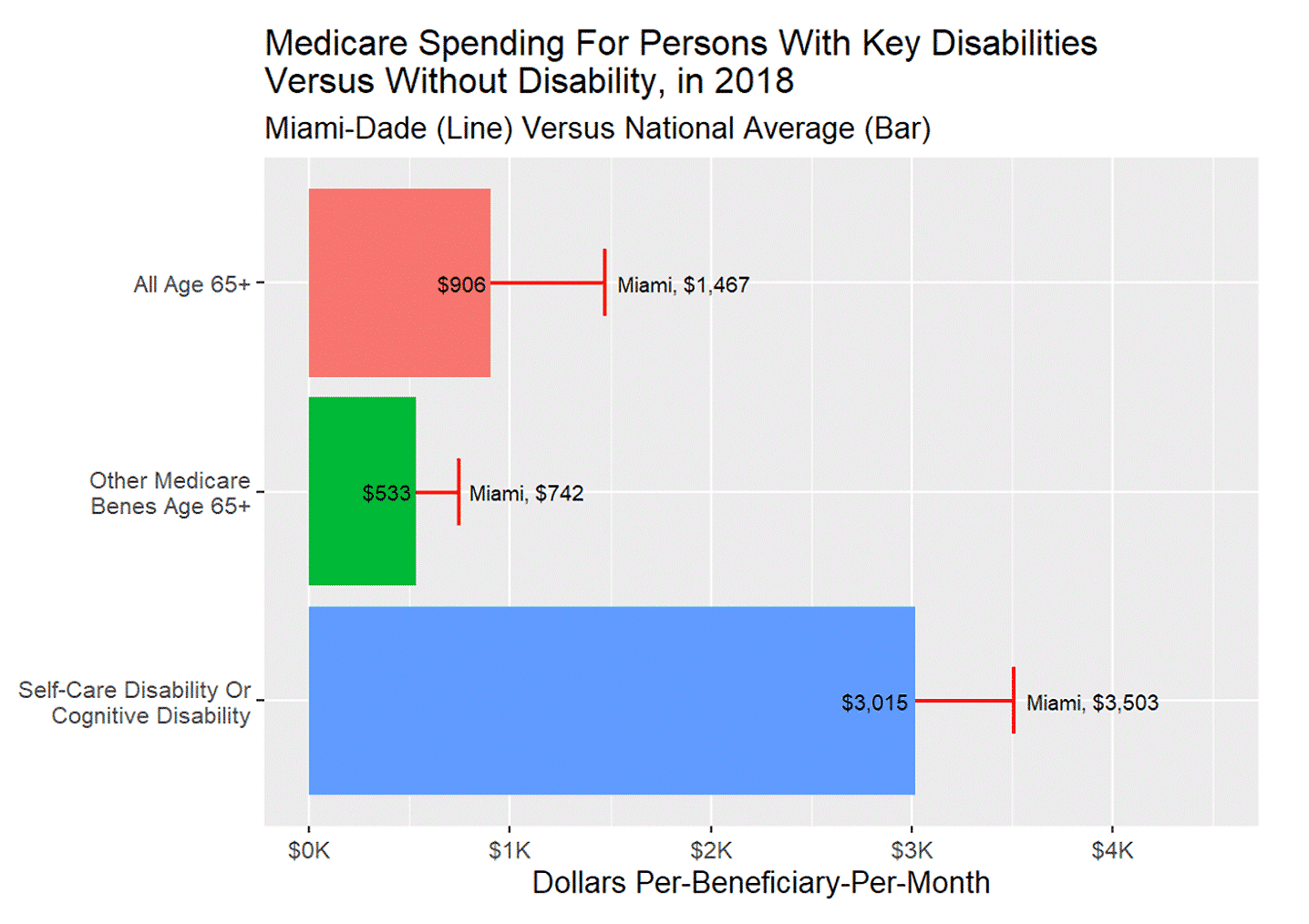
One area of interest is Miami-Dade County, Florida, home to 2.7 million persons. As illustrated in Figure 2, spending for those with self-care disability is significantly higher than the average monthly spending for the remaining age 65+ Medicare FFS population.
FIGURE 2: Demonstrating County Priorities by Comparing National Spending to Miami-Dade County Residents
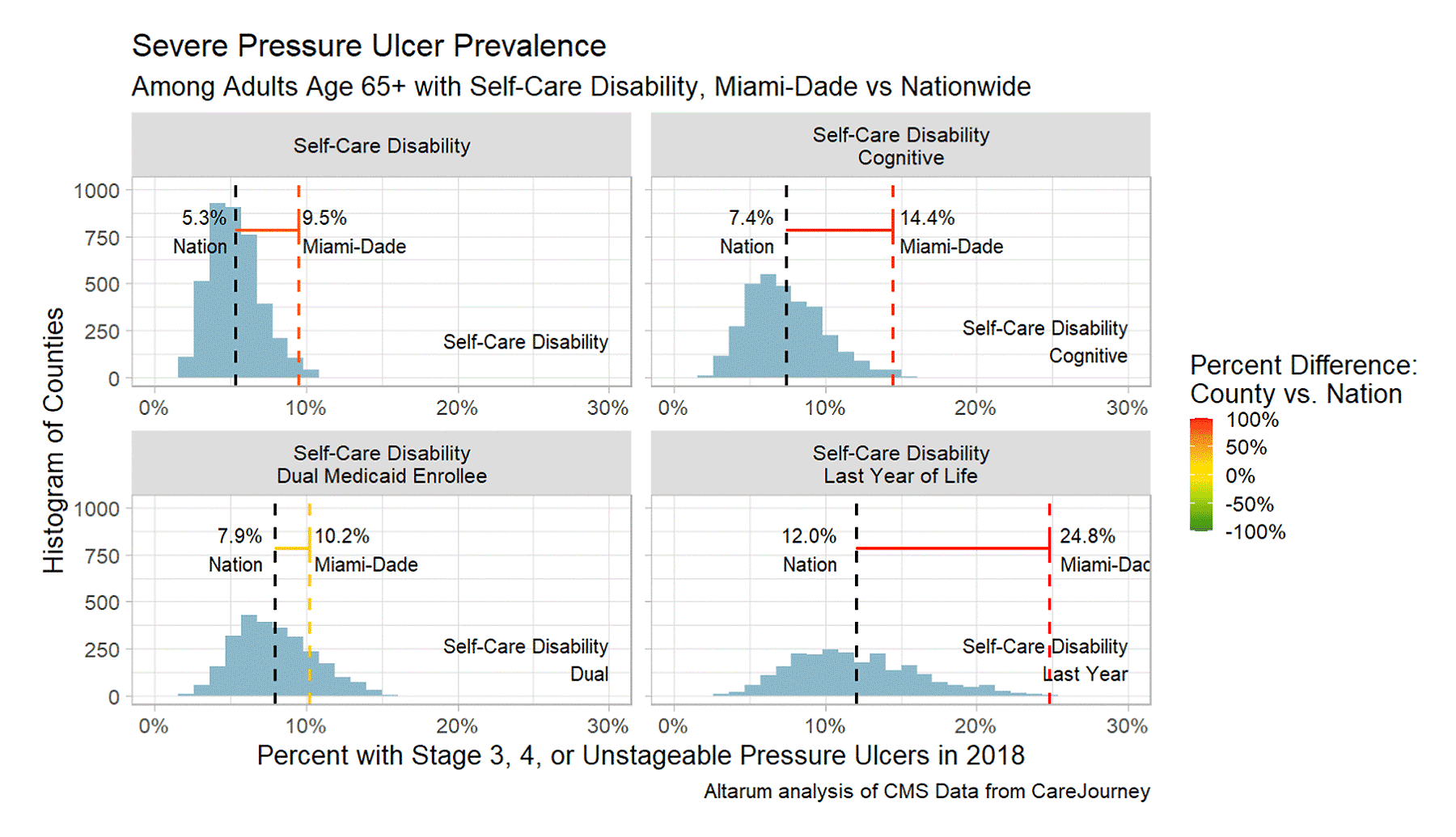
We further examined the spending for patients with self-care disability in Miami-Dade County by comparing the group to three subgroups: decedents, Medicaid enrollees, and patients with cognitive impairment. Figure 3 shows a histogram of the county distribution, with a black dashed line at the national average and a colored dashed line at Miami-Dade County’s figure.
FIGURE 3: Distributions of Medicare Spending on Key Groups, Across U.S. Counties
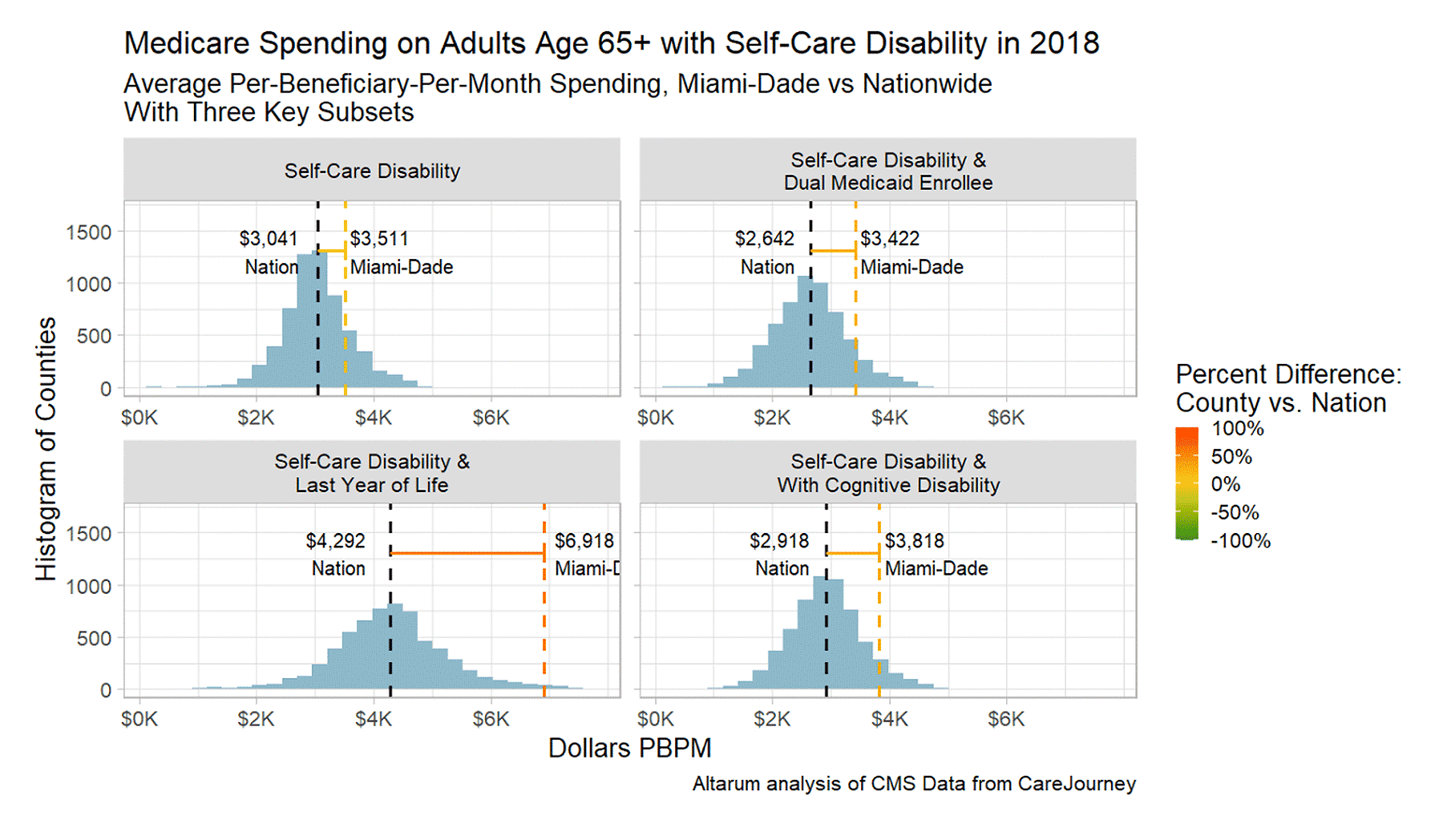
Miami-Dade falls far to the right on the “Last Year of Life” histogram. The year before death has a strong influence on Miami-Dade’s divergence from the average Medicare spending for persons with self-care disability. Nationally, in the group with self-care disability, spending is lower for those with cognitive impairment, but in Miami, the opposite is true.
Local health systems could use these data to investigate the high spending for the end-of-life experiences in this group and the experiences of those with cognitive impairment. Practice-level and health system–level analyses will reveal which organizations and their patients contribute most substantially to this phenomenon.
To further understand such high spending in Miami-Dade county, let’s examine prescribing practices and pressure ulcers. Strong studies show that both have devastating adverse consequences and can be improved with better coordinated health care.
Prescribing Practices: Benzodiazepines
Medications’ side effects in precipitating injury and impairment has spurred initiatives such as the National Institute on Aging sponsoring programs at the U.S. Deprescribing Research Network (USDeN) and the Getting the Medications Right (GTMR) Institute. The GTMR Institute promotes comprehensive medication management, and its research fellows estimated the annual cost of non-optimized medications to be $495 billion to $673 billion.
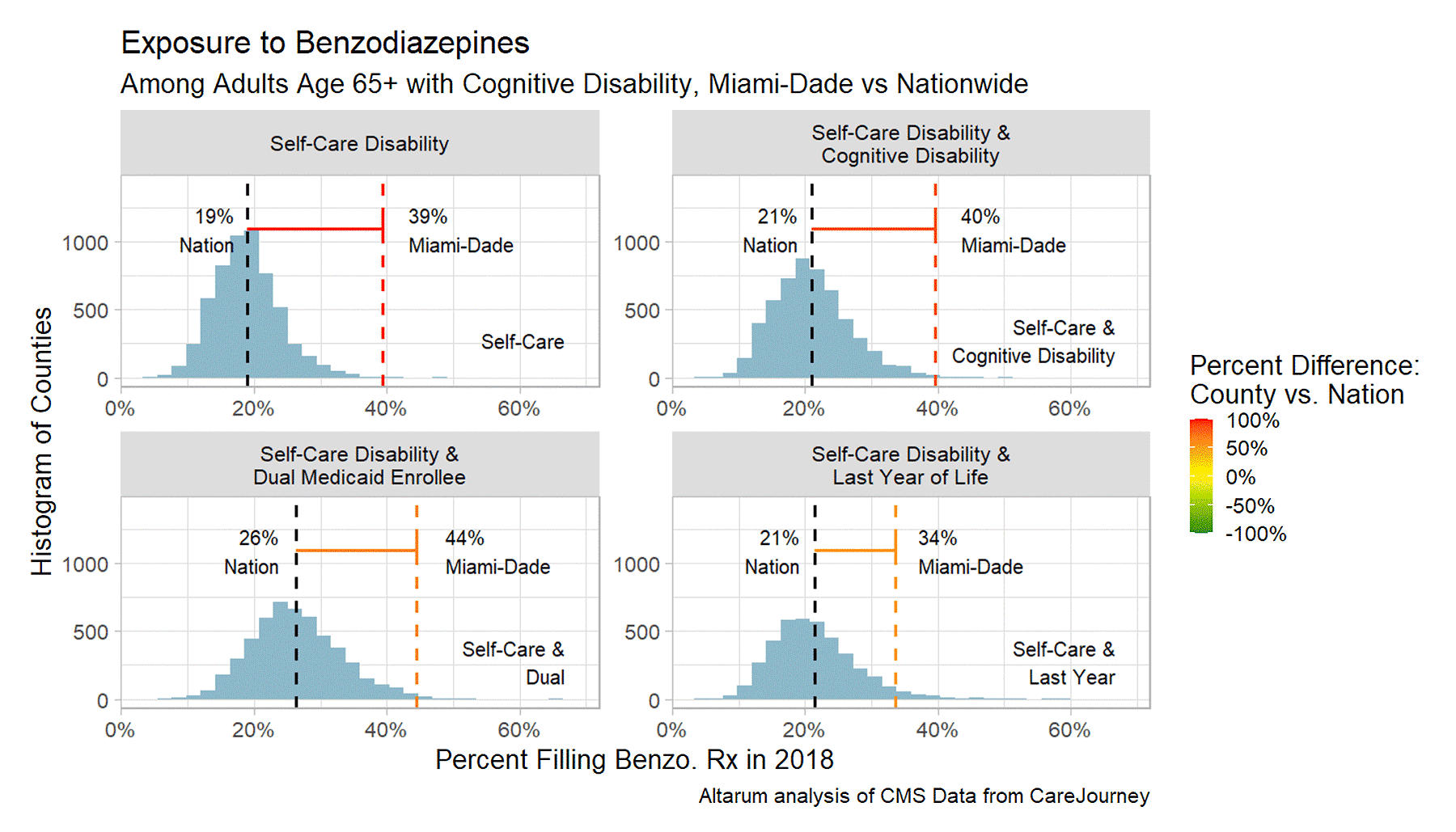
Two particular drug classes that should rarely be prescribed to elder adults are antipsychotics and benzodiazepines. CareJourney measured the number of beneficiaries filling these prescriptions in each of the impairment groups and subsets, using Part D data.
In Miami-Dade County, a shockingly high 39% of elder adults with self-care disability filled a benzodiazepine prescription in 2018. This rate was driven up by the subset of people also enrolled in Medicaid. While the national average is troubling, at 19%, it is about half the Miami-Dade rate. The American Geriatrics Society advises against any benzodiazepine prescriptions for the elderly, due to the unacceptable risk of fall-related injury, cognitive impairment, and delirium, in its Beers Criteria for drugs adverse to the elderly. We did find plenty of counties with rates half the national average, suggesting downward movement is possible through some mix of clinical or pharmacy intervention, supportive mental health services, and policy.
FIGURE 4: Distributions of Benzodiazepine Prescribing, Across U.S. Counties
Adverse Outcomes: Pressure Ulcers
Pressure ulcers are devastating by the time they reach stage 3 or 4 or cannot be staged. Research and expert opinion shows that they are both preventable and manageable, both in community settings and in nursing facilities.
Nationally in our 2018 data, one in 20 elder adults with self-care disability (5.3%) have these severe pressure ulcers, and one in eight elder adults with self-care disability (12.0%) have them in the last year of life. In Miami, the rate is approximately double on both counts (9.5% and 24.8%, respectively). This phenomenon may explain some of Miami-Dade’s exceptionally high spending on the last year of life.
FIGURE 5: Distributions of Severe Pressure Ulcers, Across U.S. Counties
Next Steps
To prioritize steps in moving to value for these key beneficiary groups, health systems require data that reveals the existing patterns of care that beneficiaries with self-care dependence and/or cognitive impairment experience. Through the collaborative work of Altarum and CareJourney, this pinpoint data is now available, with measures that highlight actionable deficiencies.
The patterns shown here – and many more, such as advance care planning and hospital discharge patterns – can be measured for the same groups, specifically those served by your system, competitors, or local long-term care providers.
Elder adults living with self-care or cognitive disabilities depend upon local arrangements for supportive services – like flexibility for family/volunteer caregiving, food delivery, personal care workforce, housing, and medical care patterns. These shape the options available to the health system and its patients. Communicating the problem to other local community leaders now can promote new arrangements, sparing the health system from confronting the painful medical repercussions of inadequate supports.
For questions about this research or how we can help, please reach us at jumpstart@carejourney.com.
About the Author
Nils Franco is a Research Analyst with Altarum, working to advance cost efficiency in the health care system by focusing on the financial valuation of public health, medical, and policy interventions.
Access the Performance Data
Fill the form on this page to access the Interactive Eldercare Performance Data.
