Background
The ongoing COVID-19 pandemic has shaken the healthcare industry dramatically. We all have loved ones affected by COVID-19 whether they are on the front-line fighting for us or they are patients trying to fight off the virus themselves. A significant focus has deservedly gone towards disease prevention and progression, but little time has been devoted to discussions around what the outlook looks like for value-based-care organizations, specifically Accountable Care Organizations (ACOs).
Before we do that, I want to highlight some of the early responses we’ve heard from a number of different health care organizations. A number of health plans have stepped up to cover the costs associated with the pandemic. We’ve seen Fresenius Medical Care and DaVita coming together to create and share a nationwide network of clinics that will focus on serving patients with COVID-19.1
We’ve also seen organizations like American Kidney Fund fund at-home dialysis for patients to comply with social distancing and remain at home to avoid disease spread – and they filled their spots within a single business day! Organizations are also releasing best practices on how to get one’s treatment while also staying safe – every little bit of this helps.
NAACOS even wrote a letter to CMS to call for adjustment to value-based payments to ensure that clinicians and ACOs were not negatively impacted by COVID-19.2 While CMS is considering these adjustments, how can ACOs be more proactive and help their clinicians that may be negatively impacted?
Fill out the form to access our special report that helps with scenario planning and understanding the potential impact of COVID-19 on your organization.
Implications for ACOs
NAACOS has estimated that the potential cost to Medicare of the COVID-19 epidemic over the next 12 months could range from $38.5 billion to $115.4 billion.3 Although CMS has invoked the MSSP extreme and uncontrollable circumstances policy in their March 30th Interim Final Rule, it doesn’t mean that ACOs are off the hook.4 This regulation will help – it states that CMS will mitigate the amount of shared losses an ACO must pay back to CMS as it relates to beneficiaries in areas impacted by the diseases (during the time of the pandemic). However, it does nothing to prevent ACOs from being forced to take on more risk in 2021 nor does it make adjustments to the benchmark or expenditures for higher than typical spending associated with these global events.4
Farzad Mostashari believes that MSSPs are prepared for COVID-19 in the way the Pathways to Success program was designed.5 He believes it protects primary care practices from most cost increases due to the outbreak. Since the Pathways program is set up so that ACOs need to perform better than the regional and national cost trends, the assumption is that everyone’s performance will rise, thereby raising the benchmark. While that will almost certainly be the case, we need our ACOs to help curb that increase as much as possible by being proactive and by reaching out to their patients that need it the most.
Potential Approaches
It’s important to note that telehealth can be provided to all patients, new and established, COVID-19 positive or negative and that the cost-sharing will be waived accordingly.6 Regardless of the stage in their value-based care journey, every ACO can do something to help their cause. In our previously released “Call To Action”, we profile several different priorities or actions that need to be taken, including “Opening up more public data”. While we at CareJourney only have a small role to play, we are doing our best to abide and are opening up additional data for you to access. By navigating to our analysis, users will be able to use the dashboard to better understand what the pandemic could cost their ACOs as it relates to Inpatient costs. We have released this so that ACOs can better understand the impact if they don’t act now. We recommend that all organizations consider the following four actions:
-
- Determine the potential impact
- Evaluate your vulnerable population
- Proactively reach out to your vulnerable populations
- Utilize your best practices
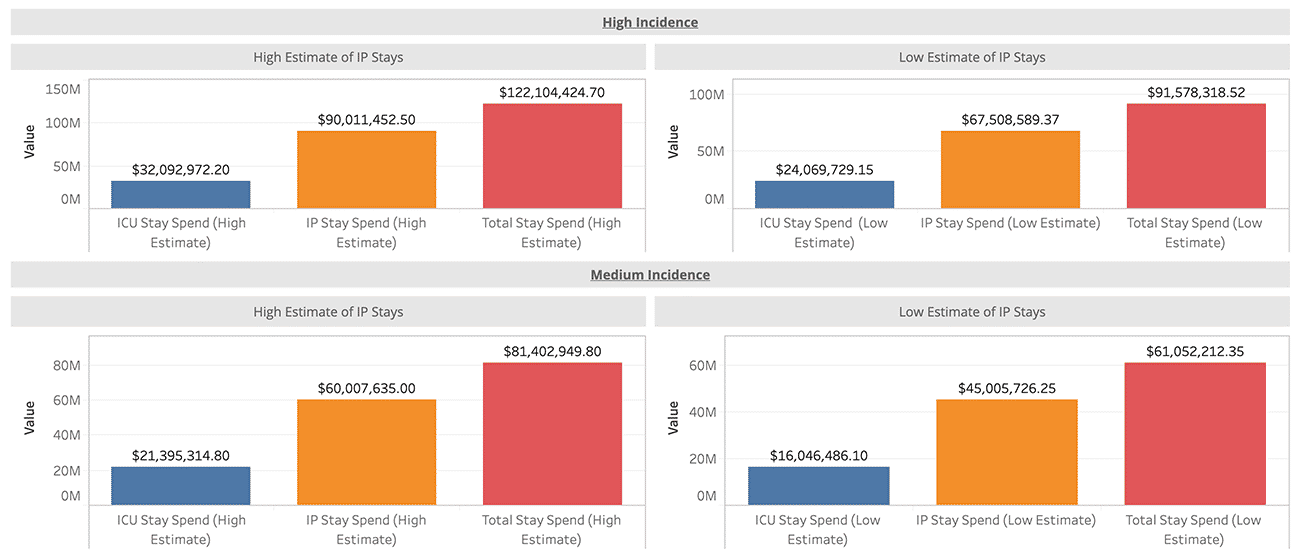
Determine the potential impact by leveraging public data to estimate the impact to your bottom line. Accounting for some assumptions from a Fair Health Article, we can assume a 20, 40, or 60% incidence rate, 50% of your affected population will seek treatment, and of that, 15% will need an Inpatient stay.6 These numbers will allow you to do various scenario planning exercises to take the next step and realize there is plenty that you can do.
Graph 1: Scenario Planning to Understand Impact to ACOs
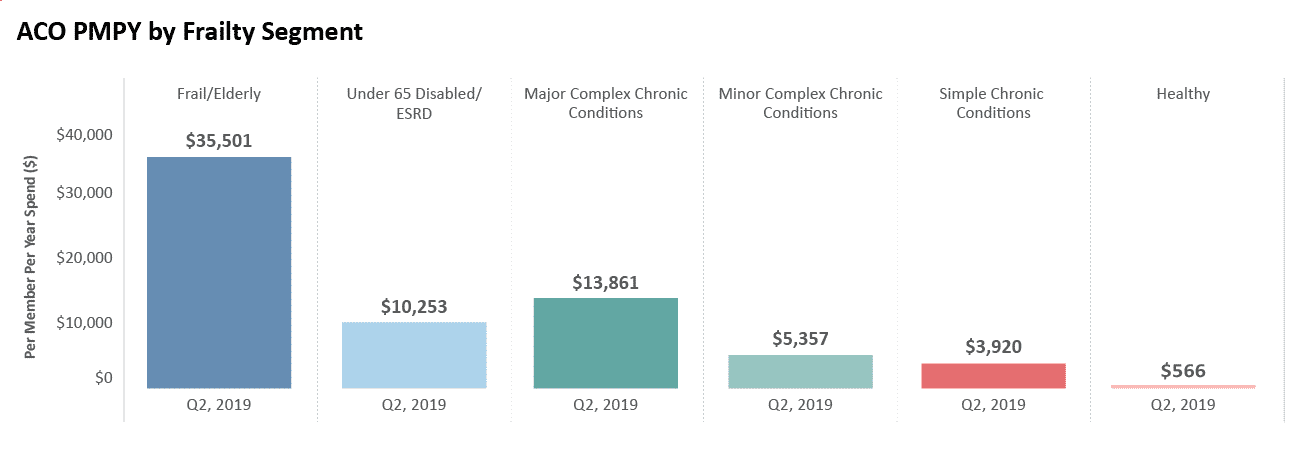
Evaluate your vulnerable population by leveraging any data to which you have access. Whether it’s our previous dashboard that uses a recently published article7 to heat map your population using the various risk factors or our collaboration with Microsoft and Dartmouth or your own claims and/or clinical data, it’s critical to understand those who may be more likely to fall ill to COVID-19. While it’s true that we will not be able to predict each beneficiary that falls ill, these data points may help you better evaluate your high-risk population to begin your outreach.
Graph 2: Example of a way to segment a population and calculate their per member per year spend, using the frail elderly algorithm developed by the Ashish Jha et al team at Harvard
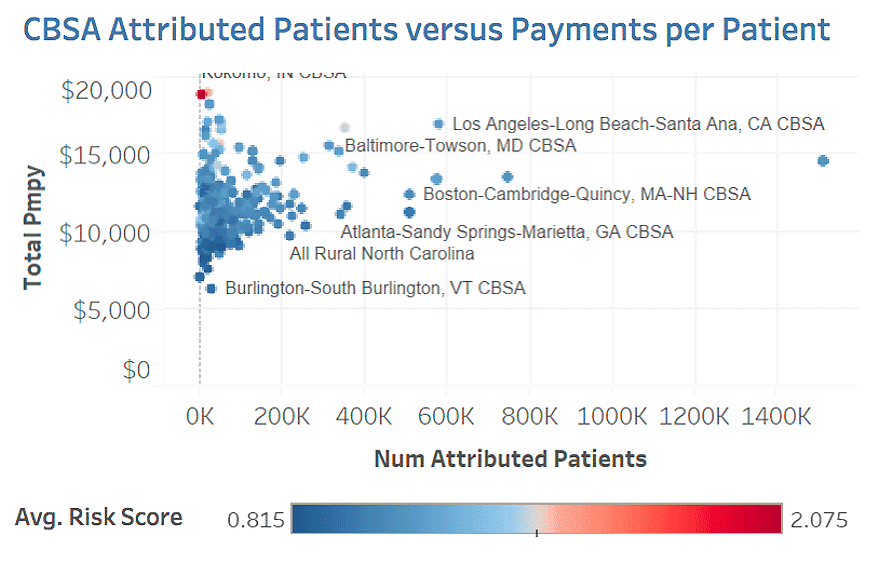
Proactively reach out to your vulnerable populations by utilizing your care managers and any other staff suited for community outreach. The staff needs to understand what resources are available to your beneficiaries and how best to reach out. Do you have EHR data and/or claims data available to you to understand who to prioritize in your outreach? Do your beneficiaries know to stay home and socially distance themselves? Do they know the community programs available to them or the telehealth options should they fall ill?
Graph 3: Profiling patients to better understand your segments/cohorts for proactive outreach
Utilize your best practices. There’s a saying “best practices are the ones that work for you”. This couldn’t be more true today. Below are two examples of best practices that we’re hearing from our members.
“No beneficiary left behind.” A member from outside Chicago has enlisted the help of our Member Services team to code up a list of criteria based on the previous dashboard to provide an actionable historical list of patients. They are then matching that list up to what they have internally to make sure they’re not leaving any beneficiary behind.
“A comprehensive, 360-Degree View.” A member in the Pacific Northwest has been working to match their claims and clinical data up to also generate a list of patients for proactive outreach. Their staff has been communicating the importance of first leveraging community resources and the benefits of telehealth before traveling to the Emergency Department unless absolutely necessary.
During a critical time like this, it’s important that all our front-line workers get as much help as they can even if that means better patient education. It is afterall for the wellbeing of not only our ACOs but our future.
Explore with CareJourney
Want to understand the impact to your ACO? CareJourney has the tools necessary to help you do exactly that. Please contact us using the link below for more information or to request a meeting.
Not a CareJourney member?
Request a demo
- Modern Healthcare. (2020). DaVita, Fresenius partner to create network of COVID-19 dialysis clinics. [online] Available at: https://www.modernhealthcare.com/providers/davita-fresenius-partner-create-network-covid-19-dialysis-clinics
- NAACOS. (2020). Leading Provider Organizations Seek Relief Through COVID-19 Response. [online] Available at: https://www.naacos.com/press-release–leading-provider-organizations-seek-relief-through-covid-19-response
- NAACOS. (2020). Potential Impact of COVID-19 on Medicare Spending: Implications for ACOs. [online] Available at: https://www.naacos.com/potential-impact-of-covid-19-on-medicare-spending–implications-for-acos
- NAACOS. (2020). COVID-19 and ACOs Fact Sheet. [online] Available at: https://www.naacos.com/covid-19-and-acos-fact-sheet
- Broome, T and Mostashari, F. (2020). “DEEP DIVE: HOW THE MSSP PROGRAM IS PREPARED FOR CRISES LIKE COVID-19” [online] Available at: https://www.aledade.com/deep-dive-how-mssp-program-prepared-crises-covid-19
- A FAIR Health Brief. (2020).The Projected Economic Impact of the COVID-19 Pandemic on the US Healthcare System. [online] Retrieved from https://s3.amazonaws.com/media2.fairhealth.org/brief/asset/COVID-19%20-%20The%20Projected%20Economic%20Impact%20of%20the%20COVID-19%20Pandemic%20on%20the%20US%20Healthcare%20System.pdf
- Zunyou Wu, MD, PhD; Jennifer M. McGoogan, PhD; Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China
