How Your Patients Benefit From Quicker Clinical Insights
By Chinmay Hunasgi
May 30, 2023
As value based payment models have evolved, so has the need to simplify and standardize the transmission, analysis and representation of healthcare data. The goal of the effort is to provide a seamless and scalable experience for providers without sacrificing data quality or security.
The Centers for Medicare & Medicaid Services (CMS) has led the effort to ensure synchronization between all of its partners. CMS has offered several APIs to distribute data more efficiently to program participants. The Beneficiary Claims Data API (BCDA) is one of the APIs that has the potential to drive significant impact with Medicare Shared Savings Accountable Care Organizations (MSSP ACOs) and REACH ACOs.
Case Study: UpStream Tracks Real-Time Provider Cost and Utilization Trends with Weekly Insights
BCDA enables organizations such as ACOs that are responsible for the care of their attributed beneficiaries to download bulk claims data for those beneficiaries. While ACOs have had access to this data in the past, BCDA offers a significant advantage in reducing the claims lag. We will delve into the specific details in the following sections.
What is BCDA?
BCDA is a data sharing platform that enables CMS to provide Medicare claims data to organizations participating in some of Medicare’s alternative payment models (APMs). These organizations use the claims data to help them improve care coordination, reduce healthcare costs, and increase the quality of care provided to Medicare beneficiaries.
Although the Beneficiary Claims Data API has been accessible for a period of time, our members have conveyed to us that few have utilized it to a significant extent or at all.
Who Can Access BCDA Data?
Access to BCDA is currently limited to participants of the Medicare Shared Savings Program (MSSP), ACO Realizing Equity, Access, and Community Health (ACO REACH), and Kidney Care Choices (KCC) models. Healthcare organizations enrolled in these APMs can grant third parties such as research organizations, app developers, and others, access to their claims data through BCDA. These organizations may be able to use the data to assist participants in care improvement initiatives.
In general, the data offered by the BCDA through CMS is an advantageous asset for diverse parties involved in the healthcare industry, facilitating enhanced care coordination, improved outcomes, and reduced costs.
On-Demand Webinar: Accelerating Insights in Value-Based Care
Learn how Pearl Health and UpStream leverage timely, patient-level BCDA analytics to improve care coordination, event notification and financial forecasting.
Earlier Claims Signal Means Better Patient Care
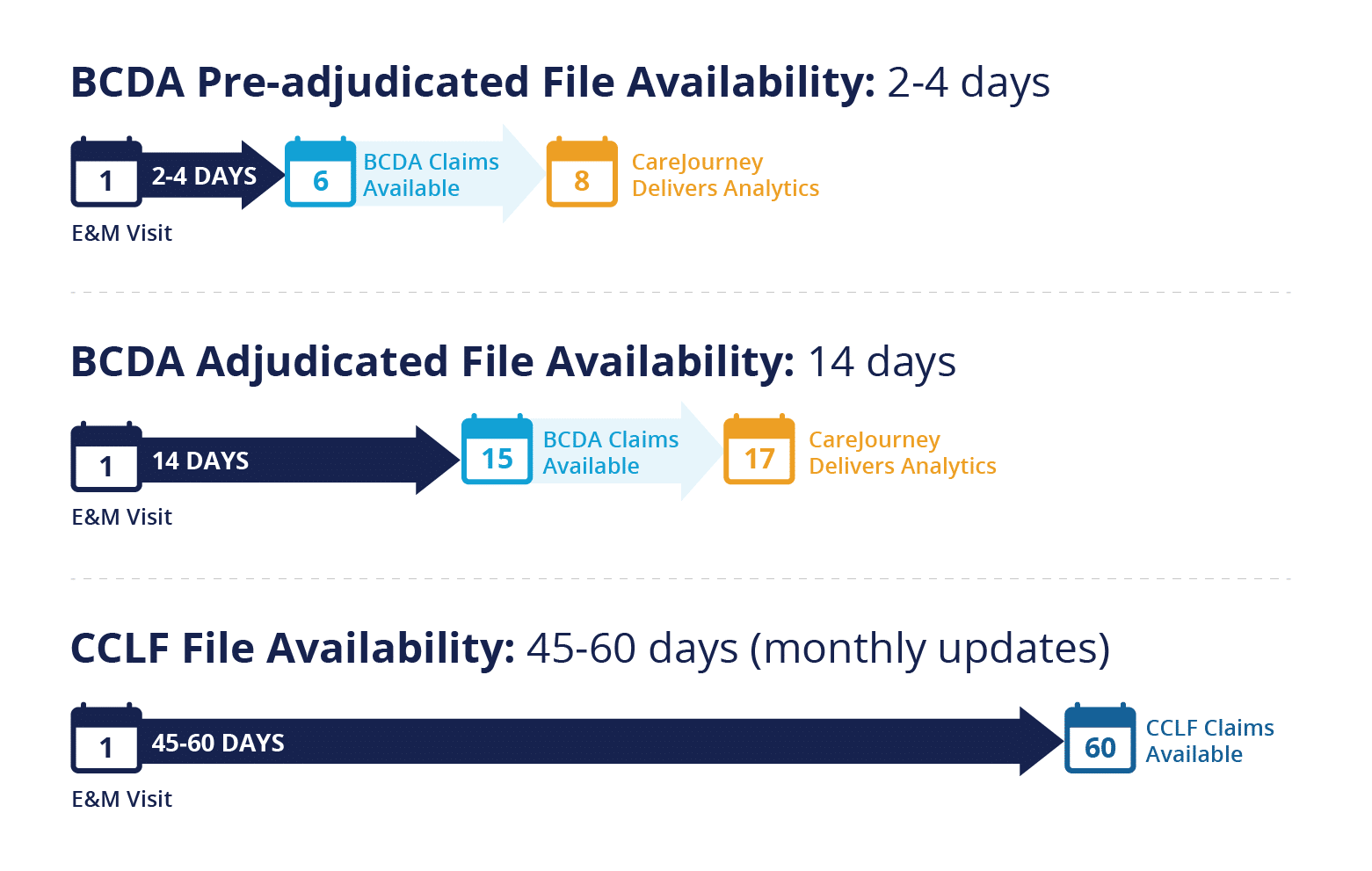
Typically, CMS takes four to six weeks post-service date to make the data available through the Claim and Claim Line Feed (CCLF). However, the BCDA offers adjudicated claims data much sooner, approximately 14 days after the claim submission, and is refreshed weekly.
Whitepaper: 6 Drivers of Success in Value-based Care
BCDA has recently introduced an enhancement for ACO REACH entities, which was in a limited release, but was pushed to production on May 16, 2023. This enhancement allows access to claims data within two to four days of their submission, providing valuable patient information, even though the claims have not been fully processed or paid and are only partially adjudicated. The data is updated on a daily basis, ensuring up-to-date information is available to users.
Imagine a situation where a patient urgently requires attention. Unlike our current system, which categorizes patients on a monthly basis, causing significant delays in providing timely interventions, BCDA’s pre-adjudicated claims data revolutionizes this process. With BCDA, we can accurately identify “red patients” (patients with multiple high need conditions) within just 2-4 days. This innovative breakthrough transforms the healthcare landscape, empowering providers to initiate timely outreach weeks (sometimes months) earlier. Providers no longer have to rely on outdated information from a month ago.
BCDA enables healthcare providers to promptly intervene and proactively address critical cases with exceptional efficiency. By utilizing BCDA-derived outputs, providers can take immediate action, resulting in enhanced patient outcomes.
Notwithstanding the aforementioned, the availability of CCLF files shall persist, albeit the BCDA affords opportunities that extend beyond the intended functionalities of CCLFs.
Breaking Down the BCDA Resources
The BCDA API delivers claims data in bulk according to the FHIR specification, utilizing five resource types: ExplanationOfBenefit (EOB), Patient, Coverage, Claim and ClaimResponse (the latter two only available via pre-adjudicated option). This differs from the CCLF files, which contain 12 files. Further information about the data can be found here.
Derive Immediate Value From BCDA With CareJourney
While having access to the BCDA is a great resource for ACOs, it doesn’t provide immediate value on its own. Users must overcome complex challenges to make it consumable and actionable. CareJourney specializes in assisting you with the following essential steps, all of which can be difficult to tackle alone:
- Sourcing and Normalizing Data: We understand the complexities of data acquisition and normalization. Our expertise ensures that you have access to high-quality, standardized data that is ready for analysis.
- Calculating Relevant Metrics and Insights: Extracting meaningful insights from raw data can be a daunting task. CareJourney’s advanced analytics capabilities enable us to derive clinically-relevant metrics and insights that are tailored to your specific needs.
- Delivering/Integrating into Operational Workflows: It’s crucial to integrate these metrics and insights seamlessly into your operational workflows to drive actionable outcomes, otherwise the insights go unused. CareJourney has built a robust infrastructure that enables a variety of delivery methods, so that you can easily integrate with your existing clinical workflows.
At CareJourney, we focus on enabling organizations participating (or thinking about participating) in value-based care to harness the power of data and analytics to succeed in alternative payment models. By partnering with CareJourney, you gain access to a comprehensive solution that utilizes BCDA data to address use cases including, but not limited to:
- Prioritizing patients, identify care gaps, and intervene in a timely manner
- Avoiding redundant testing and services by providing relevant information
- Pinpointing escalating risks before they lead to adverse events
- Uncovering coding gaps in risk scores and ensure accurate recording of diagnoses
- Leveraging an early indications of cost trajectory to hone care strategies
