How Integrated Bundles Drive High Value Specialty Care
By Keely Macmillan, M.P.H., and Erica Everhart, J.D.
July 24, 2023
Integrating episodes of care within your population health infrastructure can drive higher value specialty care and increase savings earned. While CMS aims to support more coordination between bundles and ACOs, organizations should set a specialty care strategy that works for them.
Specialty care accounts for a disproportionate share of healthcare expenditures in the US, driven in part by remarkable advancements in diagnosing, preventing, and treating serious illness. Responsible for an estimated $2 trillion dollars annually and 63% of all medical expenditures, specialty care is also a substantial source of variation in quality, outcomes, and access. This critical component of whole-person care remains fragmented and inaccessible for too many patients, particularly among younger Medicare enrollees with disabilities. To achieve meaningful progress in the transition from fee-for-service to value-based care, specialty care must be embedded within longitudinal care redesign efforts and alternative payment arrangements.
Despite its outsized relationship to low value care, specialty care has been largely peripheral to payment reform efforts to date.
Acute and chronic episodes of care offer an effective tool to identify variation in specialty care performance, optimize referrals and engage specialists in improving outcomes. For over a decade, CMS and the CMS Innovation Center have operated limited bundled payment models simultaneously with population based total cost of care models. The concurrent sets of models generally created more options for providers to transition to value-based care and have led to critical learnings and favorable results in certain types of episodes. However, to date, the overall impact of episodic models including Bundled Payment for Care Improvement (BPCI), BPCI Advanced, Comprehensive Care for Joint Replacement and the Oncology Care Model have not yielded transformative improvements in quality or cumulative savings to Medicare. Further, the asynchronous and overlapping nature of the different programs has led to complications with attribution, benchmark setting, savings allocation, and specialist engagement.
An estimated 75% of low-value care is neither provided by nor referred by the beneficiary’s attributed primary care provider.
In its recent RFI, CMS reiterated its goal to increase specialist participation in accountable care and the need to change how episode-based models “coexist” with ACOs. CMS also shared more insight into the agency’s plans to test a new, mandatory bundled payment model that would go into effect no earlier than 2026 and incentivize coordination between care settings. CMS anticipates the new model would be narrower in clinical scope than BPCI Advanced and with shorter episode lengths. The model would require participation by entities in selected geographical areas, and CMS’ future data transparency initiatives would aim to equip ACOs with better insights to manage specialty care. CMS requested feedback on a wide range of questions, including how to ensure future models advance health equity.
While CMS’ future goal for more coordinated models is welcome, organizations with population-level, total cost of care accountability are already well positioned to integrate episodes of care within their existing longitudinal care infrastructure. ACOs, clinically integrated networks, and provider systems in risk contracts with Medicare Advantage or commercial payers would all be well-advantaged to align high value specialists with their primary care foundation through “shadow” bundles. Implemented for an aligned patient population and run independently of CMS, shadow bundles are defined by a discrete set of services and are triggered when an attributed patient experiences specific acute events or chronic conditions. Shadow bundles may vary in length and scope depending on clinical condition, site of service and course of treatment, and are attributed to specialists who are accountable for the patient’s cost and quality of care for the episode of care. Because shadow bundles are implemented within a total cost of care model, specialists are incentivized to coordinate with longitudinal care providers across the continuum to enable person-centered care. Through this integrated model, shadow bundles help accelerate performance and enable greater savings payments, particularly under more sophisticated benchmarking methodologies that use administratively set benchmarks.
Shadow Bundle Assessment and Planning
Through a claims-based assessment, an at-risk provider organization can understand the volume, expenditures, and variation in cost and quality associated with different clinical disease categories affecting their patient population and among specialists in and out of their network. Newer organizations focused on growing and optimizing their networks could use this information to identify high value specialists for referrals. Organizations focused on improving performance could use insights including opportunity for savings and levers for quality improvement to prioritize key bundles for its shadow bundle program.
For example, if an ACO identified that its patient population had a sizable amount of spending associated with hip replacements, a significant amount of variation in episodic performance among orthopedic surgeons and opportunities to optimize post acute care utilization and reduce complications compared to peer benchmarks, hip replacements would be a good candidate for shadow bundle implementation.
Hip replacements are an example of an acute episode in which an orthopedic specialist would be accountable for the procedure and would coordinate with longitudinal care providers for post acute, follow up and maintenance care. The Duke Margolis Center for Health Policy figure below illustrates how episodes of care can be integrated within a patient care journey.
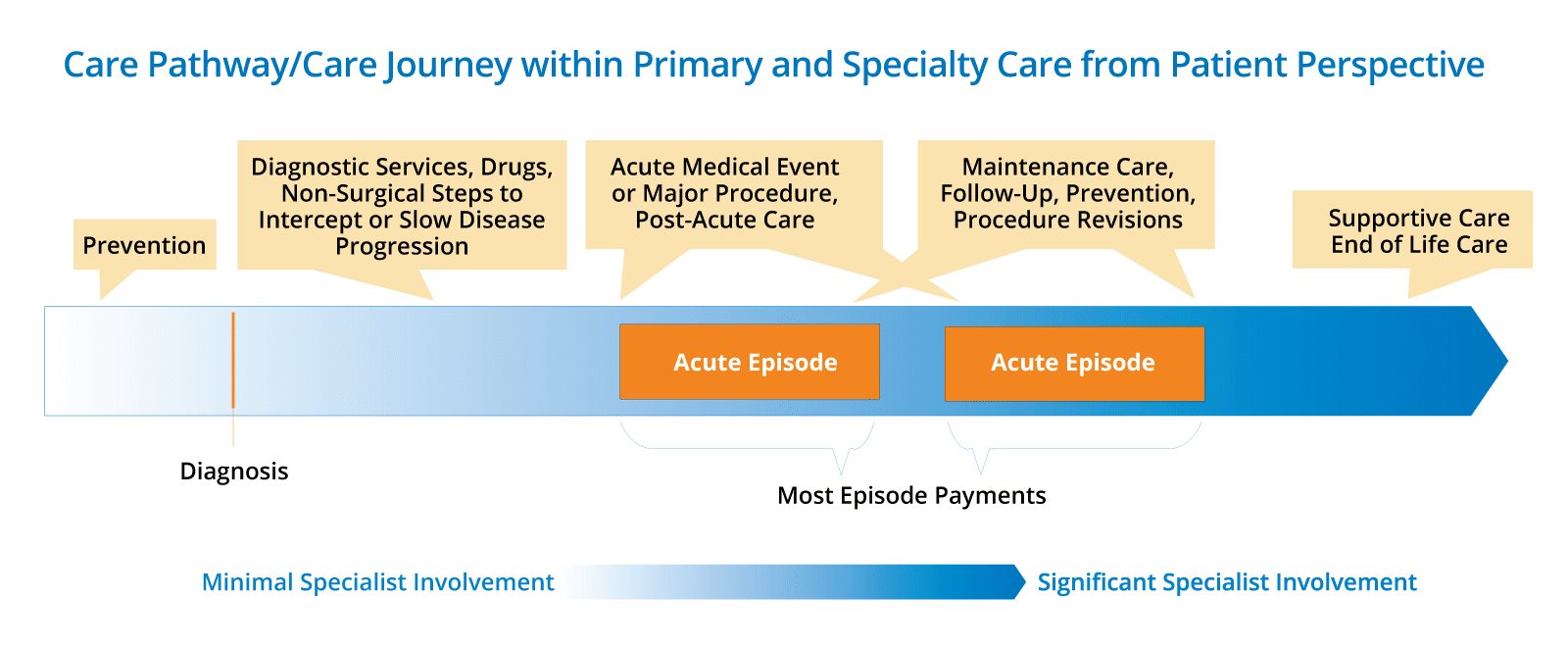
Image credit: The Duke Margolis Center for Health Policy, Strengthening Specialist Participation in Comprehensive Care through Condition-Based Payment Reforms
As part of the shadow bundle program, the ACO would select orthopedic surgeons for participation, set meaningful financial and quality targets, and leverage HIT, risk assessment tools, care coordination, a preferred post acute care provider network, and other value-based care tenants to support a coordinated care journey.
Depending on an organization’s legal structure and payer contract arrangement, incentive payments with orthopedic surgeons could be structured through a range of funds flow mechanisms including prospective capitated payments, distributions from a shared savings pool, and bonus payments based on quality performance metrics. With more proposed cuts to physician reimbursement, performance-based payments under risk arrangements may be the only avenue for some physicians to earn greater revenue under Medicare.
Part two of this blog showcases how CareJourney data can be used to identify and prioritize episodes with opportunity.
Key Takeaways
- CMS will continue to play a critical role in the adoption of value-based care, however, providers should set their own strategies for aligning high value specialists.
- At-risk organizations can use episodes of care and peer comparisons to identify variation in specialty care, optimize referrals and set meaningful targets for improvement.
- Controlling the referral faucet is an extremely valuable lever for ACOs, and shadow bundles are another valuable tool to align cost and quality incentives across providers.
- Coordinating acute and chronic bundles with longitudinal care providers can accelerate performance and increase shared savings payments in accountable care models.
ACO Specialty Care Analysis: Orthopedic Surgeons by Cost and Quality
Read the next blog in this series to learn how to select episodes with opportunities for performance improvement.
How CareJourney Can Help
CareJourney is rolling out enhancements to its Provider Performance Index including refinements to 300+ high potential episodes of care across dozens of clinical specialties. Constructed from Medicare and commercial data, episodes are risk adjusted and attributed at the physician, group, facility and TIN level to quantify opportunity for any ACO, CIN or system and help organizations identify the optimal specialists to manage episodes of care. Risk-adjusted, outcome-based quality metrics are calculated for all episodes across specialties including orthopedics, oncology, behavioral health, endocrinology, nephrology, and pulmonology. Peer benchmarks can help organizations identify meaningful targets for improvement and effective financial incentives to engage specialists.
