By Vinith Annam
Creating Patient Risk Groups
In a previous blog post titled Harnessing Open Health Data & Methodologies to Serve Value-based Care Networks, CareJourney discussed Harvard T.H. Chan School of Public Health’s development of a publically available patient segmentation model which identifies a small percentage of Medicare beneficiaries who account for a majority of an Accountable Care Organization’s (ACO) spend. Given its ability to better target an ACO’s costliest patients for purposes of savings, CareJourney incorporated Harvard’s segmentation model into Insights Online. A cross-collaborative effort such as this is one example of how CareJourney is committed to opening itself to adoption of care models across partners.
In that spirit, CareJourney has closely worked with South Texas Clinical Partners ACO (STCP), an organization owned and operated by Universal Health Services (UHS) and managed by Imperium Health, to implement a care model of their own.
Conceptually analogous to Harvard’s formation of clinically relevant patient groups, STCP has created a method of assigning patients to risk groups for identifying current and emerging high need-high cost beneficiaries. In addition, the ACO has formed interventions for each risk group to improve care management.
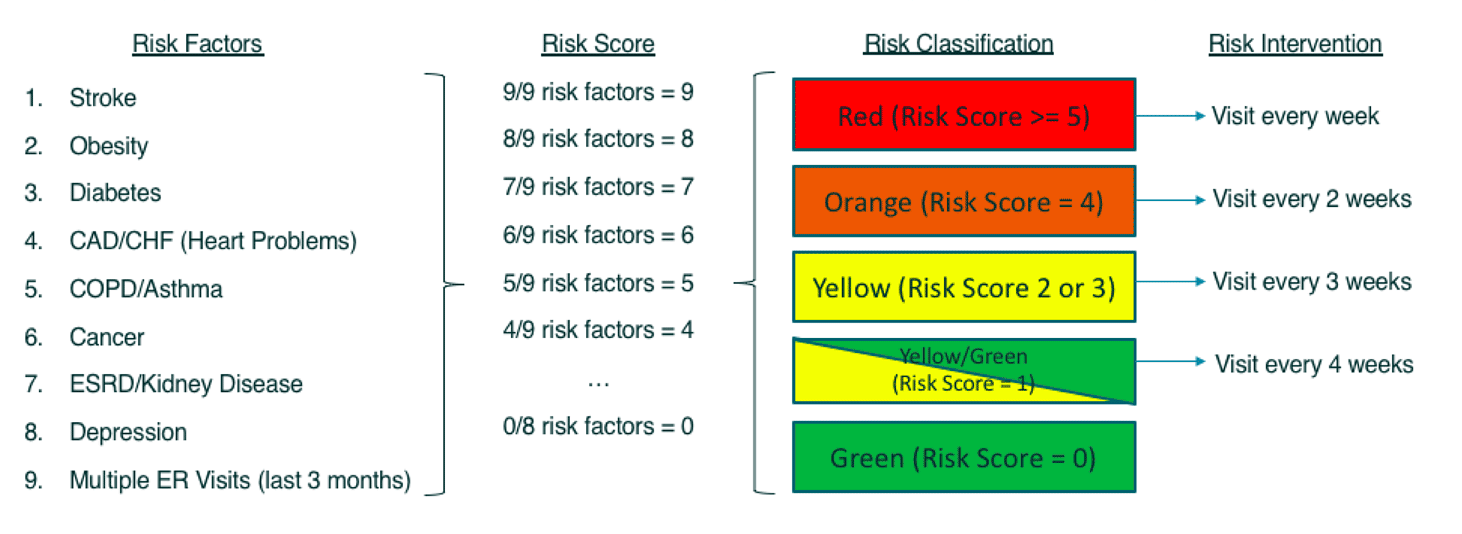
Dr. Monzer Yazji, STCP ACO’s Chief Medical Officer, developed the rules which determine a patient’s risk group assignment and his/her corresponding intervention. CareJourney obtained Dr. Yazji’s rules illustrated below, translated its logic into code, and processed this logic against claims data to assist STCP in creating actionable patient dashboards and worklists.
STCP Patient Risk Group Model
Dr. Yazji’s risk classification and intervention methodologies are described below:
- For each patient, observe 9 factors to determine which risk group he/she belongs to. 8 factors are chronic conditions as defined by CMS’ Chronic Conditions Data Warehouse (click herefor link). 1 factor is multiple ER visits (at least 2 visits within past 90 days).
- Count number of concurrent factors a patient has at a moment in time to derive a risk score. Each individual factor is worth 1 point (e.g. 3 concurrent factors = risk score of 3, 4 concurrent factors = risk score of 4, etc).
- After calculating a tallied risk score, assign patients to risk groups ranging from green (risk score of 0) to red (risk score of at least 5).
- Determine PCP intervention frequency based on risk group a patient belongs to. This ranges from a visit every 4 weeks for a yellow/green patient to once-a-week for a red patient.
Making Patient Risk Groups Actionable
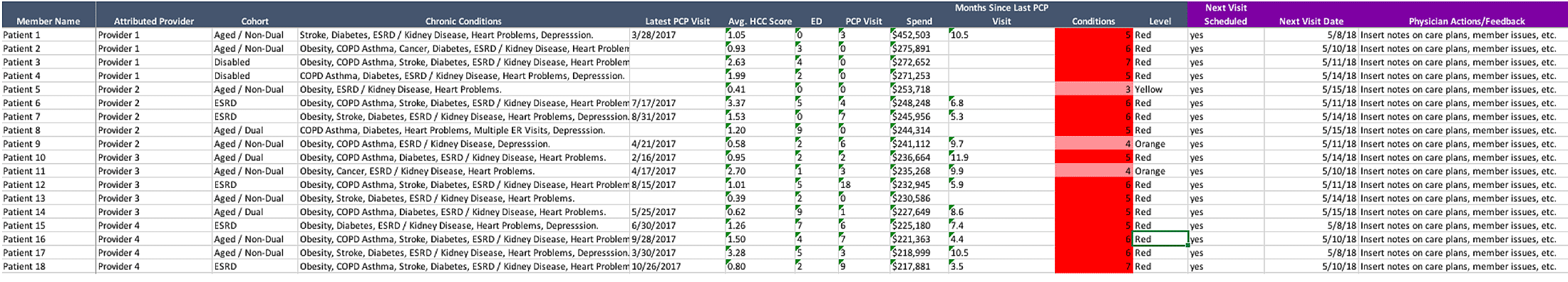
It is worth noting that CareJourney’s product development process allows for flexibility in adjusting UHS’ algorithm logic. For example, users can request incorporation of additional chronic conditions, assign different weights on those chronic conditions to create a new scoring system, and revise their approach to risk grouping. After processing claims data through UHS’ segmentation logic, care managers share patient worklists with physicians such as the one below (all information is fictitious for illustration purposes). Column headers in purple are where physicians/practices enter manual notes – specifically when a patient should have their next PCP visit as well as any other additional noteworthy details. This process has tremendously helped STCP coordinate care for its thousands of patients.
Summary
Collaboration between CareJourney and UHS has brought claims data to life, giving care managers and providers better knowledge on how they can capture “low hanging fruit” for greater ACO savings. Given that there are still tremendous opportunities for an ACO to lower costs while improving care quality, CareJourney is continually crowdsourcing ideas as well as sharing its knowledge and insights with clients. Please don’t hesitate to contact us with thoughts or questions – we look forward to hearing from you!