Application of a High-Need Patient Segmentation Framework in ACOs: A Research Collaborative Between ACOs, the Harvard T.H. Chan School of Public Health, and CareJourney
Brief Background:
In recent years, the shift towards value based care, especially in ACOs, has increased provider accountability for growing healthcare costs. As such, clinical leaders of ACOs need data-driven approaches to identify potentially modifiable sources of high healthcare spending among their attributed population. One compelling strategy for managing rising costs is to focus on the group of patients that are at risk for being high-cost over time. These high-need, high-cost (HN/HC) patients are not a monolithic population, and thus, there is a need to better characterize these patients into subpopulations for more effective targeting.
Recently, a research team at the Harvard T.H. Chan School of Public Health defined six “segments” of the Medicare HN/HC population: the non-elderly disabled, frail elderly, major complex chronic, minor complex chronic, simple chronic, and the relatively healthy (Joynt et al, Healthcare, 2017). This work was informed and shaped by the National Academy of Medicine. Using these segments, we found tremendous heterogeneity in the HN/HC patient population. For example, the frail elders were far more likely to be HN/HC than any other subpopulation. Among the frail elderly, post-acute care was a major driver of costs while prescription drugs were the largest source of spending among the non-elderly disabled. There was also large variation in potentially preventable spending across Medicare subpopulations, with the majority of preventable spending concentrated among the frail elderly for conditions like bacterial pneumonia and urinary tract infections (Figueroa et al, Annals of Internal Med, 2017).
Although our work was instrumental in shaping definitions of HN/HC populations, the next crucial step is to apply this framework in real-world clinical settings, refine it, and improve it to ensure we can drive meaningful changes in the care for HN/HC patients.
The Project:
HSPH is seeking 10 ACOs to partner and apply the HN/HC segmentation framework to their data. Participation in this collaboration will offer key insights into how your ACO is managing specific HN/HC subpopulations. ACOs will also gain an understanding on what proportion of their spending on HN/HC subpopulations is potentially preventable or deemed potentially a “low-value” service.
ACOs that choose to participate in this collaboration will have the HN/HC segmentation framework applied to their Medicare data. Application of the HN/HC framework will be done by CareJourney and, with the CareJourney member’s permission, a representative from the HSPH team will be granted access to their Medicare CCLF data housed by CareJourney as a subcontractor to conduct analyses on the applied framework.
Over the course of 12 months, the HSPH team will seek feedback from ACOs about alternative ways to view their data and seek feedback on how to refine the HN/HC subpopulations. The objective is to improve and refine the HN/HC segmentation framework to be used as a tool for tracking HN/HC patients and assist with the development of programs and interventions to improve their care.
Application of the HN/HC Segmentation Framework:
Application of the segmentation statistical code to CCLF file data will identify 6 Medicare subpopulations within each ACO. These include the the frail elderly, the non-elderly disabled, the major complex chronic, the minor complex chronic, the simple chronic, and the relatively healthy (See Figure 1).
Figure 1. Medicare subpopulations
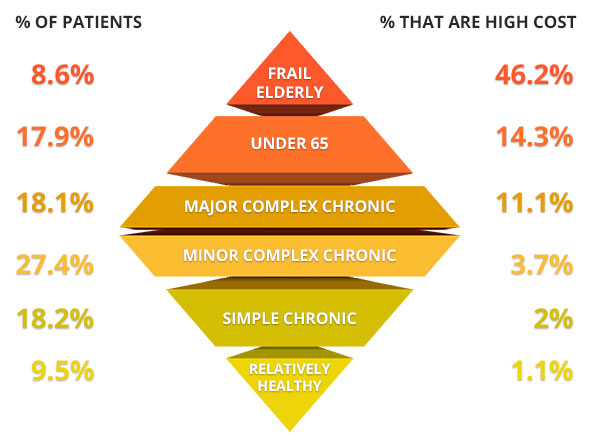
Joynt, K.E., Healthcare (2016), http://dx.doi.org/10.1016/j.hjdsi.2016.11.002.
Next, we will examine the levels of spending and utilization by each subpopulation from every participating ACO. To calculate spending of each participating ACO, we will use claims data from the CCLF files to determine spending in following areas: inpatient, outpatient, carrier, post acute (including skilled- nursing facilities, rehabs, and home health), and drugs. We will use standardized costs, to allow for fair comparisons across ACOs and to national benchmark independent of differences in regional prices. Standardized costs will be calculated using the CMS method, where we assign costs for each type of service based on a national Medicare rate. In addition, we will determine what proportion of spending is potentially preventable. This will include spending related to acute care services for ambulatory care sensitive conditions (e.g. admissions for urinary tract infections, dehydration, etc.) and low value-services (e.g. colorectal cancer screening in adults over the age 85).
Seeking Feedback from ACOs on how to improve the HN/HC Segmentation Framework:
After the initial application of the segmentation work to participating ACOs data, we plan to seek feedback on the utility of this approach during the first 6 months of the project from ACO participants. Specifically, we will seek input on what information they gained is useful and what’s not useful. We will also seek input on other ways ACOs would want to view data on high-need patients. Information gained from this phase will then inform how the HSPH team will improve and refine the HN/HC segmentation framework.
Data Protection:
ACO data will remain in the CareJourney environment. ACO data including patient information will not be shared with others except with the individual ACO. Publicly shared findings will not be reported at the ACO-level, only in aggregation with other participating ACOs. Unless requested otherwise, the ACO will be named as a participant in the collaborative. The HSPH team will eventually apply the refined HN/HC Segmentation Framework to an anonymized national Medicare sample. The algorithm or the code-book developed in collaboration with ACOs will be made public for others to use.
