Advance Care Planning: Disparities Between MA and FFS Enrolled Medicare Beneficiaries
Nate Smith, PhD – CareJourney, Tatiana Fofanova, PhD – Koda Health, and Desh Mohan, MD – Koda Health
November 3, 2022
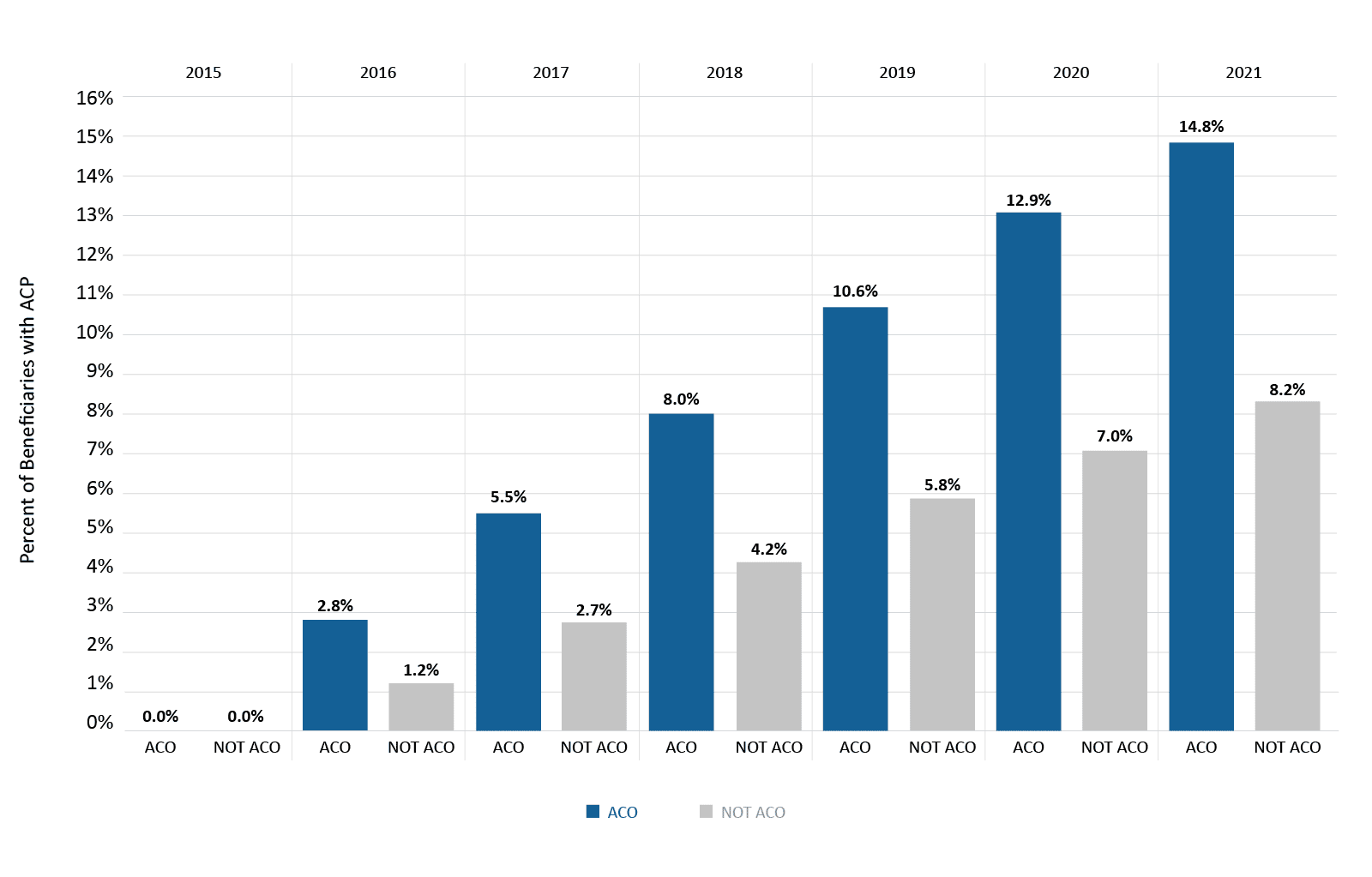
CareJourney and Koda Health today announced new findings on the adoption rate of Advance Care Planning (ACP)1, using Medicare claims and enrollment data from 2015 to 2019.2 Overall, adoption rates of ACP are sluggish, with significant disparities across race and dual-status between Medicare Advantage (MA) and Fee-for-Service (FFS) beneficiaries. However, Accountable Care Organizations (ACOs) are administering ACP at higher rates among FFS beneficiaries, and at higher rates compared to MA beneficiaries.
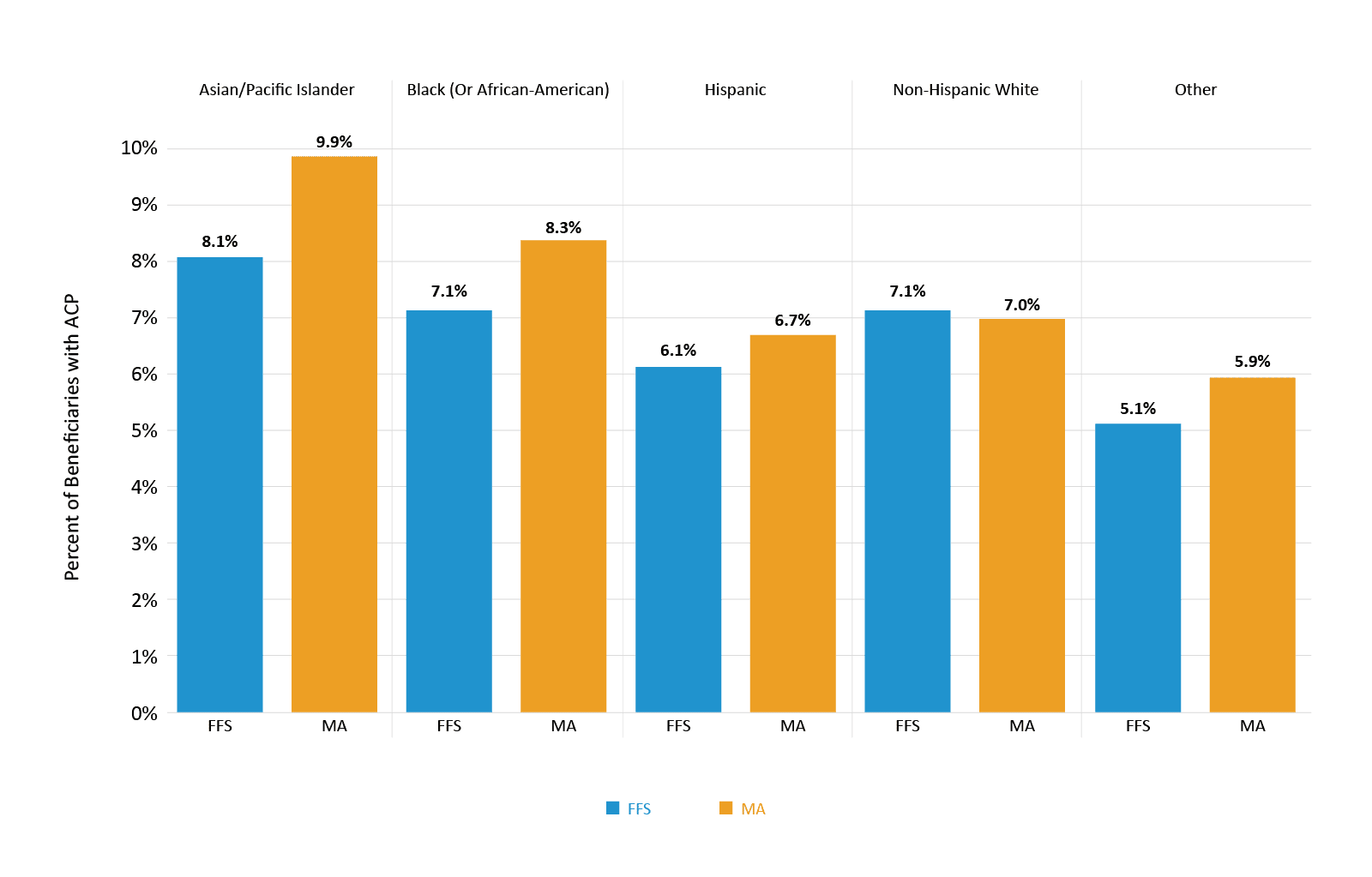
Similar to prior studies, the analysis found that fewer than 7.2% of Medicare beneficiaries engaged in ACP overall as of 2019. However, minority populations, including Black/African-American (8.3% vs 7.1%), Hispanic (6.7% vs 6.1%), and Asian/Pacific-Islander beneficiaries (9.9% vs 8.1%) had higher levels of engagement when enrolled in MA rather than FFS. “Recent studies have shown that many physicians avoid these conversations with folks that don’t look like them,” says Dr. Tatiana Fofanova, CEO of Koda Health, “so it’s encouraging to see the MA approach slowly closing this disparity.”
Advance Care Planning is the process that supports adults at any age or stage of health in understanding and sharing their personal values, life goals, and preferences regarding future medical care.
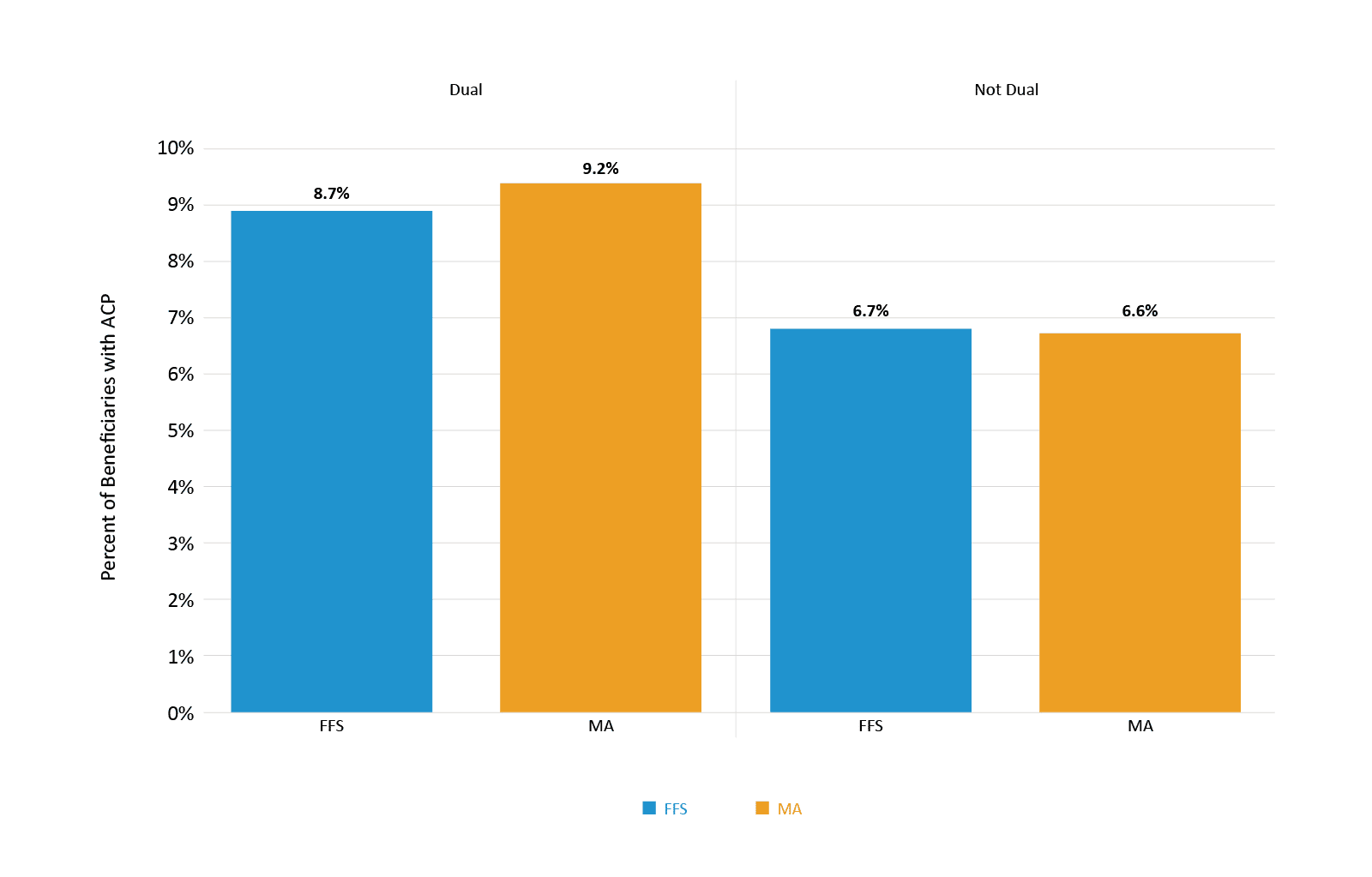
Furthermore, dual-eligibles (9.2% vs 8.7%) were more likely to be engaged in ACP if they were a MA beneficiary rather than FFS. (Figure 1 and 2). Many Medicare beneficiaries live at or below the poverty line, and yet, they have historically spent more of their income on healthcare than the wealthiest 1/3rd of beneficiaries. It’s well documented that the oldest and the poorest are the highest utilizers of healthcare – due, in no small part, to a lack of access to proactive healthcare planning. This analysis suggests that MA plans are making progress in closing this equity-of-access gap, at least in terms of ACP.
Value-based care arrangements overall appear to be leading the charge on ACP. Beneficiaries who were part of an ACO were 1.8 times more likely to have been engaged in ACP than those beneficiaries not attributed to an ACO. (Figure 3)
“These are difficult conversations to have and those patients who need it the most often aren’t engaged by the healthcare system. Providers often have limited time, are uncomfortable guiding care planning conversations, and frequently lack tools to effectively document patient preferences into legal documents like advance directives,” says Dr. Desh Mohan, Chief Medical Officer at Koda Health.
“It is well known that there are inequities in access to this important conversation and process,” says Dr. Fofanova. “This data highlights a silver lining that we are beginning to see across the industry. Value-driven healthcare organizations, like ACOs and MA, are beginning to understand the importance of Advance Care Planning in driving better health outcomes and quality of life for patients regardless of their background.”
In line with these findings, Aledade recently announced the results of their three-year study on the impact of Advance Care Planning, which demonstrated an impressive $13,916 in reduced costs per patient over an average of 14 months. Furthermore, new bipartisan legislation introduced in September aims to expand ACP access, in line with the Biden Administration’s prioritization of ACP in CMS settings.
While billing is important when measuring ACP, there are also other components that are indicators of the quality and value of ACP and end-of-life care initiatives. “Beyond the checkbox of a billing code or completed advance directive, it’s important to build and measure a process that promotes thoughtful planning among patients, their care team, and their loved ones,” says Dr. Mohan.
CareJourney and Koda Health are excited to collaborate to help improve benchmarking data for Advance Care Planning and end-of-life metrics. Koda Health is a leader in delivering high-quality, equity-driven ACP at scale to healthcare organizations, and will be providing clinical and practice-based expertise to guide the construction of toolkits, dashboards, and benchmarks that improve ACP programs and end-of-life outcomes.
“Integrating beneficiary goals within a care plan, particularly on difficult end-of-life decisions, should be a bedrock objective for value-based care organizations,” noted Aneesh Chopra, CareJourney’s co-founder and President. “I’m hopeful next-generation quality measures will honor the patient’s voice in defining what it means to deliver high quality care, and our commitment is to measure progress on that important endeavor.”
About CareJourney
More than 140 customers trust CareJourney as the healthcare industry’s best source of provider cost and quality data. CareJourney’s cloud-based analytics platform helps value-based care organizations build and grow networks, improve provider performance, identify network integrity and strengthen referrals, and better manage at-risk populations.
About Koda Health
Koda Health builds tools that simplify difficult conversations in healthcare. Clinically validated and research-driven, Koda’s flagship ACP software platform provides payors and providers the ability to engage their patients in valuable conversations about their care preferences. Through Koda, patients have a single source to explore their values, identify a surrogate decision maker, define their quality of life, indicate treatments that matter, and complete and share advance directives — all without burdening their care team. By working with health systems and health plans, Koda increases revenue for billing providers, drives cost savings for at-risk systems, and ultimately is able to offer their services to patients completely for free.
For more information on Koda Health, visit http://www.kodahealthcare.com or contact info@kodahealthcare.com
- Numerous studies have shown that ACP ensures patients’ preferences are fulfilled, decreases burden and anxiety among loved ones, improves patient quality of life and satisfaction, decreases unwanted medical utilization, and appropriately increases palliative and hospice utilization. Recognizing the impact of ACP, CMS introduced ACP billing codes in 2015 to incentivize adoption in the clinical setting.
- ACP reimbursement by Medicare began starting January 1, 2016. KFF Fact Sheet
