ACOs and Rural Healthcare
By Chris Lester and Sabrina Chugani
June 22, 2018
Roughly 20 percent of the United States population lives in rural areas. Despite this, rural America faces a number of health-related challenges, some of which are structural, while some are related to regional differences in health and health care in this country. Compounding these issues, incomes are lower and poverty rates are higher in many rural areas (USDA, 2018).
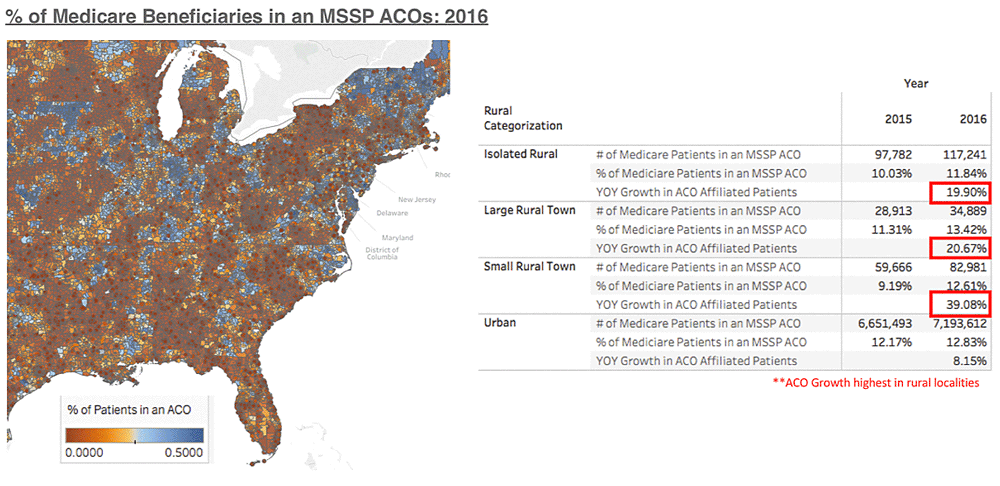
In a recent analysis, we found that most MSSP covered lives occur in urban environments, but the largest relative growth (analyzing 2015 against 2016) has actually occurred in rural areas.
Despite rapid growth in recent years, when diving in deeper to assess rural ACO financial performance, the numbers did not necessarily show the same trend. Rural ACOs tended to have worse financial performance and worse care model coordination than urban ACOs.
| % of Patients in a Rural Setting | Average TCM Compliance | Average AWV Compliance |
|---|---|---|
| 0%-2% | 11.41% | 34.33% |
| 2%-10% | 9.79% | 27.75% |
| 10%-20% | 9.67% | 26.41% |
| 20%+ | 4.15% | 23.97% |
Additionally, for those ACOs in rural settings, they tended to have a more difficult time achieving shared savings. Per the table below, in 2016 there were 8 ACOs with more than 20% of patients living in a rural setting. Of those 8, only 3 made savings and the average savings rate was -1.13%.
Interestingly enough, ACOs with a predominantly rural population actually had the highest average quality score.
| % of Patients in a Rural Setting | Number of ACOs | Number of ACOs that Made Savings | Average Savings Rate | Average Quality Score |
|---|---|---|---|---|
| 0%-2% | 382 | 196 | 1.22% | 94% |
| 2%-10% | 90 | 21 | -0.18% | 96% |
| 10%-20% | 32 | 5 | -0.89% | 97% |
| 20%+ | 8 | 3 | -1.13% | 99% |
When drilling into the NPI level to better understand performance and the high quality scores we observed for these rural ACOs, we found that NPIs affiliated with ACOs in rural areas are vastly superior to their counterparts outside of ACOs in basic care management – per the data in the tables below, we observed that rural ACOs are caring for rural patients better than they would be otherwise.
AWV Compliance for PCPs in 2016
| In an ACO? | Isolated Rural | Large Rural Town | Small Rural Town | Urban |
|---|---|---|---|---|
| Yes | 38.3% | 61.3% | 20.4% | 32.4% |
| No | 7.2% | 19.5% | 10.9% | 23.0% |
TCM Compliance for PCPs in 2016
| In an ACO? | Isolated Rural | Large Rural Town | Small Rural Town | Urban |
|---|---|---|---|---|
| Yes | 9.5% | 10.4% | 7.9% | 10.1% |
| No | 4.5% | 4.1% | 4.8% | 6.2% |
In summary, there are many compelling reasons for developing ACOs in rural areas. Care coordination, teaching patients about their medications, and management of disease states have shown significant increases in the quality of care and quality of life for patients served by the ACO as evidenced by the data presented above.
If you’d like to see a more recent analysis, check out our report and findings on what drives high performance in the Medicare Shared Savings Program.
References:
https://www.ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/
