Provider Data: How it Can Make or Break Your Value-based Care Strategy
By Joe Mercado, MBA, MS
October 6, 2023
Your patient needs a referral to an orthopedic surgeon. You aren’t sure who to recommend off the top of your head. You start by logging into your internal data tools and find helpful metrics on some providers, but it’s not comprehensive of all providers in your network and market. It’s hard to tell who the best physician is for this specific patient. Should you refer based on total patients seen? By patient review? Or by search result order?
In the rapidly evolving world of healthcare, data has emerged as the catalyst for transformation; however, this is a common scenario. Among the myriad of datasets that healthcare stakeholders rely on, CareJourney’s provider performance data and analytics stand out as a game-changer in situations like the one described above, providing relevant, timely, comparative, and accurate data, when referral decisions have powerful financial and clinical impacts on patients and providers. In this blog post, we’ll delve into why provider intelligence and analytics are critical and why those without these data assets risk being left in the dust.
The Power of Provider Intelligence Data
Provider intelligence data refers to the wealth of information collected and analyzed to evaluate how healthcare providers are performing. This data encompasses a wide range of metrics, from clinical outcomes, patient experiences, cost-efficiency, and adherence to best practices. The power of provider intelligence data lies in its ability to drive positive change in healthcare in the following ways:
- Quality Improvement: Identify areas where healthcare providers excel and where improvement is needed. Provider data serves as a compass guiding quality improvement efforts, ultimately enhancing patient outcomes and safety.
- Patient-Centered Care: Empower providers to deliver care tailored to individual patient needs and preferences, fostering a patient-centered approach that enhances patient experiences and satisfaction.
- Cost Reduction: Promote cost-effective practices, reduce unnecessary procedures, and lower healthcare costs while maintaining, and even improving, quality of care.
- Resource Optimization: Allocate resources efficiently by pinpointing high-performing providers and departments, optimizing staffing, equipment, and facility investments.
Across these four use cases, the stakes are high. Networks are formed. Routing decisions are made. And most importantly, patients are impacted. Without the right data, the effect can be detrimental.
The Building Blocks of Provider Profiling: Provider Intelligence
What exactly constitutes provider data? In working with 140+ organizations across a variety of sectors, CareJourney found common questions:
Which physicians are providing care? What practices and facilities are they affiliated with? What do they specialize in? How many patients do they see? Whom do they share patients with? And most importantly: are they good? Please note that CareJourney uses the word provider to describe performance at multiple levels, including group, facility, and physician.
To address these questions, CareJourney built comprehensive provider profiles and referral relationship mappings across Medicare FFS and commercial data, oriented across the following domains:
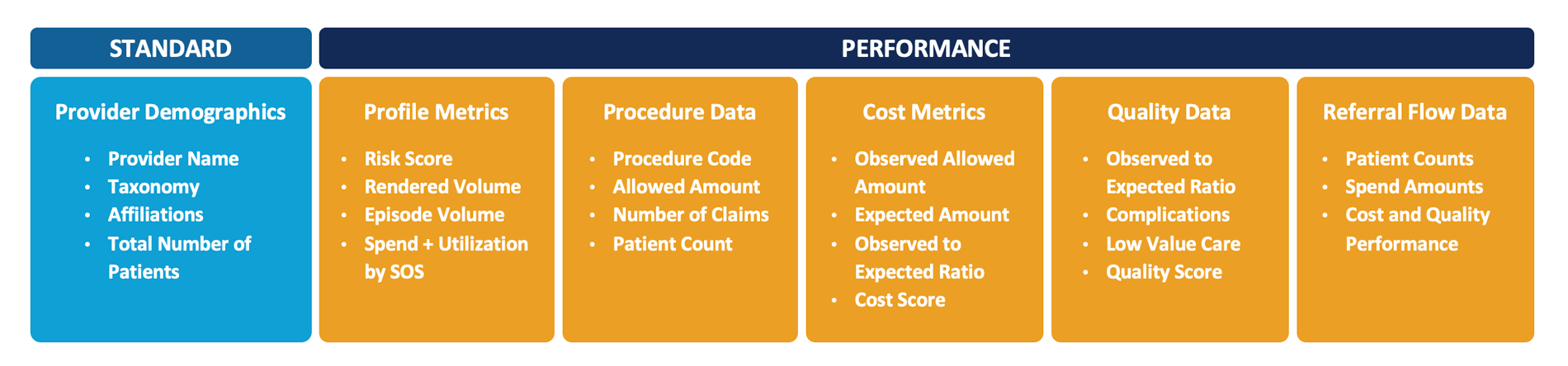
- Provider Demographics: Provider demographics, affiliations, and specialization.
- Profile Metrics: Derived insights around patient mix, sites of service, and other utilization metrics.
- Procedure Data: Spend and volume measures by diagnosis and procedure to understand treatment patterns.
- Cost Metrics: Episodic based performance data to summarize experience, cost, and utilization.
- Quality Metrics: Quality and outcomes performance data in addition to complication costs to understand provider quality, low-value care, and population care.
- Referral Flow: Provider’s patient flow in spend and volume outlining relationships between provider groups.
With this data available in bits and pieces, the challenge becomes: what comprises complete, high-quality provider data, that elevates your strategy?
The Definition of a Provider
Often, groups define a provider as the set of NPIs treating a patient. However, this is a limiting view, as there are many different entities with important variations across the patient journey.
CMS defines a healthcare provider as “a person who is trained and licensed to give health care. Also, a place that is licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers.” Given this, CareJourney defines a provider as a physician, a physician group, or facility.
We do this as a means of providing the building blocks to understand care variation across the entire continuum and unlock the opportunities to advance value-based care. This offers innovative organizations the ability to pivot their way through provider data to unearth the root of a problem, instead of jumping to the wrong conclusion.
The Categories of Provider Performance
While it’s true that there is no “one size fits all” way to measure provider performance, CareJourney has found a consensus across four key categories of performance.

- High Volume: There is an undoubtable positive correlation between procedure volume and outcomes in surgery, suggesting that provider experience is a key factor in delivering high-quality healthcare.
- Cost Efficiency: By optimizing cost efficiency, providers ensure all resources are used wisely and effectively balance cost with the delivery of high-quality care.
- High Quality: Ensuring network and affiliate providers practice with the highest quality standards is critical to your organization’s wellbeing, as well as your patients’ health and safety.
- Appropriate: Keeping patients at the forefront, high performing providers stay away from low-value or wasteful services.
Across these categories, CareJourney’s provider intelligence data includes only the relevant data needed to drive strategies forward, instead of lingering behind.
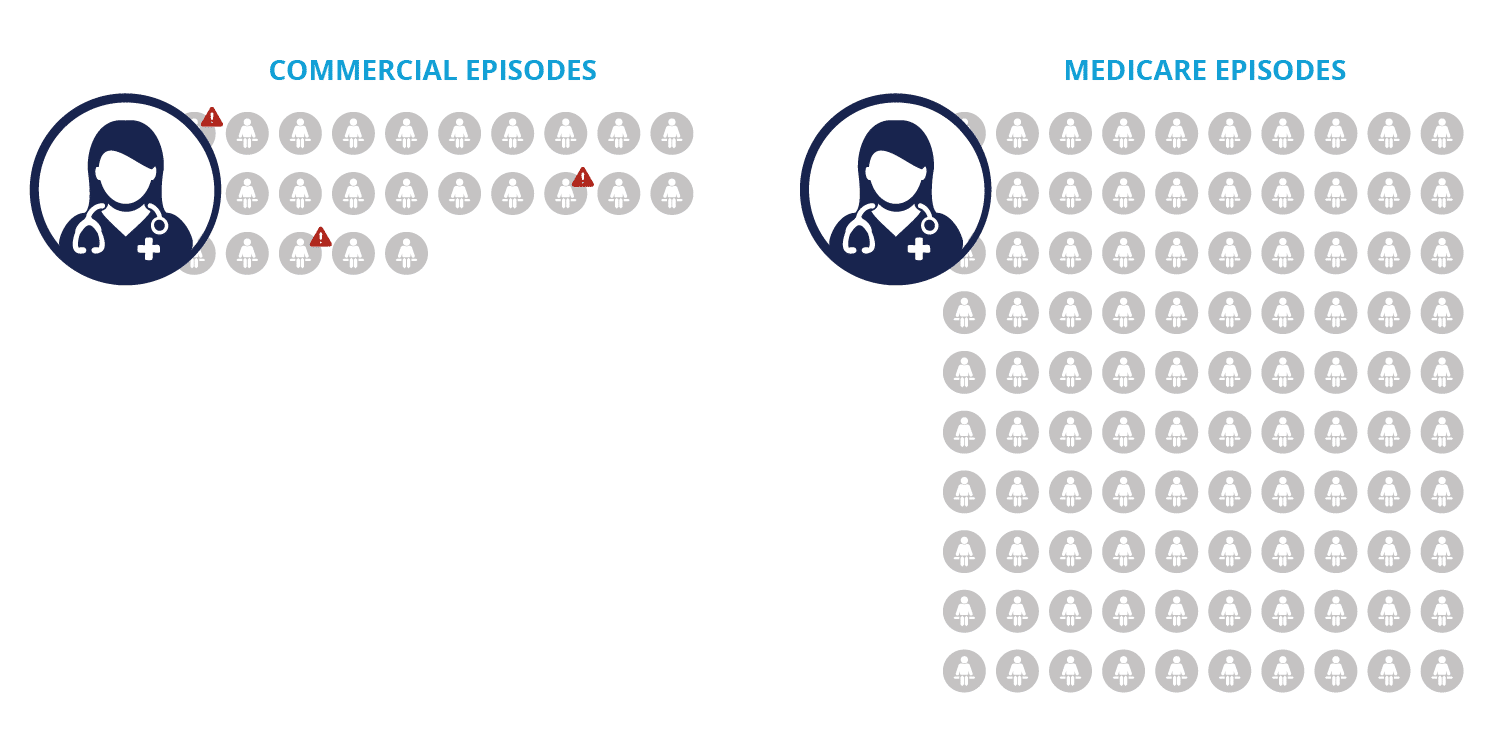
Evaluating Providers Across Multiple Lines of Business
A final key component to provider data is accurate comparisons. Doing this right requires significant investments in risk adjustment and peer comparisons which we will get into in a later piece during this series. In addition to risk adjustment and peer comparisons, it’s important to look across multiple lines of business. While some may assume that practice patterns remain consistent, having access or evaluating on a single line of business is fraught with issues. For instance, focusing on just one line of business limits the providers available for comparison (i.e., limited Geriatrics in Commercial, limited OBGYNs in Medicare) and gives some providers an unfair comparison point. Let’s say a provider does 25 episodes on a commercial population but does 100 episodes on Medicare. Let’s also say the 25 episodes include several cases that negatively impact performance. If you look at just the Commercial analytics, you miss the larger picture and if you focus on the Medicare analysis, you may ignore a flag on this provider.
Using comprehensive claims data across multiple lines of business, provider intelligence generates valuable insights that hold true across all lines of business.
Stay Ahead of the Curve with Provider Performance Data and Analytics
In conclusion, provider data and analytics are critical to success in today’s healthcare landscape. Organizations embracing the right provider data position themselves for success by fostering quality improvement, enhancing patient care, and ensuring financial viability. In contrast, those operating with partial or obscured data risk being left in the dust as healthcare rapidly continues its transformation into a data-driven, value-based industry. The choice is clear: adapt and thrive or risk falling behind. Next, read about the specific elements of provider performance analytics that are critical to success.
How CareJourney Can Help Get You Started
With access to a large national dataset of commercial, Medicare and Medicaid claims, CareJourney developed a set of comprehensive provider profiles led by cost and quality metrics and their building blocks to enable care improvement and network development use cases. Grounded in taxonomy and Provider Performance Index, our analytics include provider demographic details to maximize your strategies.

