Background
The Medicare Shared Savings Program (MSSP) is the largest value based care program from the Center for Medicare & Medicaid Services (CMS) to date. Since its inception in 2012, Accountable Care Organization (ACO) participation has doubled; providing care to over 10 million beneficiaries, generating $1.94 billion in total savings, and earning over $1.47 billion in shared savings in the latest 2019 performance year (PY).1 The purpose of this program is for ACOs to coordinate the following:
- Promote accountability for a patient population
- Coordinate items and services so patients get the right care at the right time, while avoiding unnecessary duplication of services and preventing medical errors
- Encourage investment in high quality and efficient services
So, how can we map overall savings back to the goals of the program? Is there a formula for success ACOs can unlock to ensure top tier performance in MSSP?
The answers to these questions can be very complex given all of the contributing factors. ACOs need to consider not only the patient population they are serving, but the entire market including provider network selection, health system saturation, and geographic landscape.
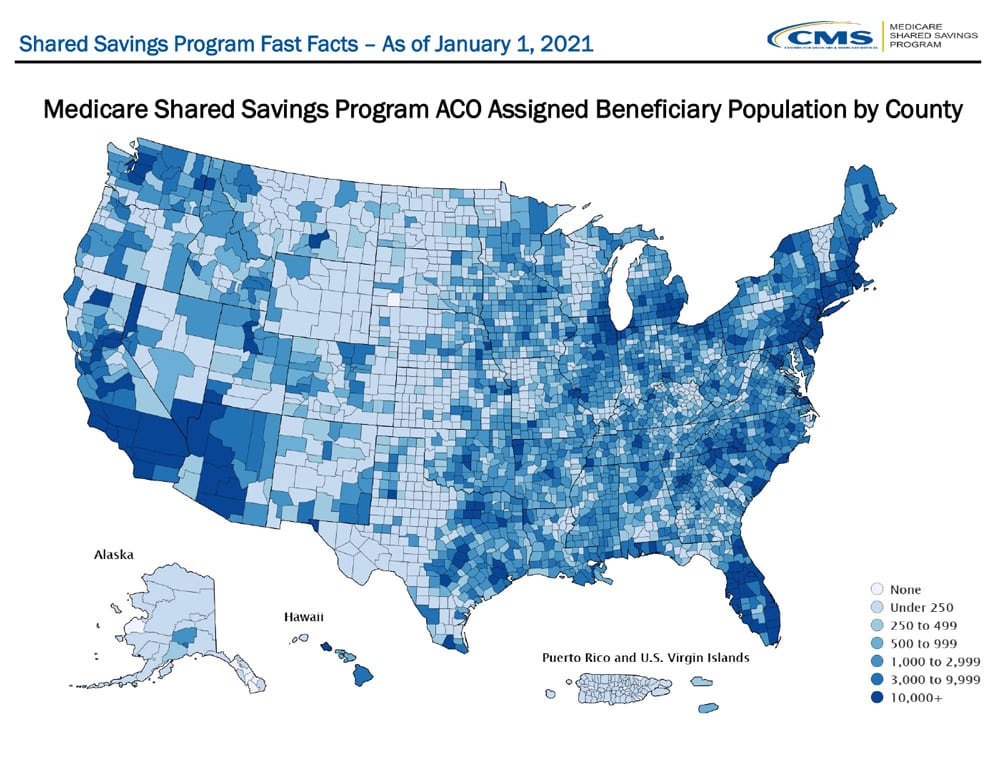
Figure 1: CMS 2021 Shared Savings Program Fast Facts. MSSP Assigned Beneficiary Population by County
There are also countless approaches and strategies to implementing value based care initiatives: What types of care coordination programs should we implement, and for which segments of our population? What is the most appropriate post acute pathway post-discharge? Are we routing patients towards the highest value specialists? Finding the right levers to pull that impact the greatest change for their populations is key to succeeding in MSSP.
Even with all of these unknowns, we continue to see “All Stars” that generate higher caliber savings year over year. 2019 was the largest annual savings to date, and the third consecutive year in net positive savings for the MSSP program.2 In fact, earned savings per ACO increased by 40% from 2018 to 2019. We wanted to better understand the ACOs that are most successful, and identify trends in cost and utilization data that could contribute to high savings.
See over 200+ cost, utilization, and quality metrics paired with total and per capita generated savings.
Profiling ACO Success: At a Glance
Leveraging CareJourney’s 100% Medicare Fee-for-Service claims dataset, we analyzed available MSSP performance results from the last three years (2017 – 2019). We evaluated over 200+ cost, utilization and quality metrics paired with total and per capita generated savings from over 450+ ACO participants. In order to sift through all of this data, we created a quintile of savings for ACOs with full year participation in 2019.
| 2019 MSSP Performance Results: ACOs Quintiled by Total Savings per Beneficiary | ||
|---|---|---|
| ACOs Ranked by Total Savings per capita | Avg Total Savings per Capita | Avg Number of Assigned Beneficiaries |
| Top 20% | $934.78 | 14,392 |
 |
$478.10 | 22,116 |
| $281.19 | 28,119 | |
| $68.34 | 25,367 | |
| Bottom 20% | $(320.05) | 17,665 |
Figure 2: CareJourney 2019 MSSP Performance Results Analysis: ACOs Quintiled by Total Savings per Beneficiary
Note that this analysis is based on total savings per capita (benchmark minus expenditures) versus shared savings earned by the ACO. In 2019 74% of ACOs generated savings for Medicare FFS, but only 55% earned savings back as part of their unique risk sharing formula. By using total savings instead of earned savings as our “KPI”, we were able to control for outside factors that impact an ACO’s “take home” value; such as quality score, risk model, savings rate etc. This allowed us to profile ACOs based solely on their savings performance in the program, and seek to understand “All Stars” through claims behavior.
Key Findings
- Experience in MSSP: ACOs with higher savings per capita participated longer in MSSP
- High vs Low Revenue: 73% of ACOs in the top quintile of savings per capita are low revenue organizations
- Risk Type: The top tiers of ACOs based on savings per capita had a higher prevalence of taking on downside risk, relative to the lower tier ACOs that were almost exclusively upside only
| 2019 MSSP Performance Results: ACOs Quintiled by Total Savings per Beneficiary | |||||
|---|---|---|---|---|---|
| Revenue Type | Risk Model | ||||
| ACOs Ranked by Total Savings per capita | Avg Years in MSSP | % High Revenue Revenue | % Low Revenue | % One-Sided | % Two-Sided |
| Top 20% | 5.21 | 27% | 73% | 78% | 22% |
 |
4.58 | 52% | 48% | 74% | 26% |
| 4.27 | 53% | 47% | 78% | 22% | |
| 3.97 | 72% | 28% | 82% | 18% | |
| Bottom 20% | 3.68 | 72% | 28% | 94% | 6% |
Figure 3: CareJourney 2019 MSSP Performance Results Analysis: ACOs Quintiled by Total Savings per Beneficiary
As you can see in Figure 3 above, on average top performing ACOs have participated in the program 29% longer than their peers with the lowest savings. This is consistent with what’s observed in the industry as it can take time to navigate, implement and realize the return on various care reform initiatives.
In addition, 73% of top performing ACOs are low revenue, which is consistent with CMS findings, and noted as their reason to create the high and low revenue designations for Pathways to Success: ‘Further, we have observed that low revenue ACOs (which are typically composed of physician practices and rural hospitals) outperform high revenue ACOs (typically ACOs that include hospitals). However, participation in performance-based risk Tracks remains modest, and some low revenue ACOs lack a pathway to transition from a one-sided model to more modest levels of performance-based risk.’3 Conversely, we found higher rates of both low revenue ACOs and two-sided risk models in top quintile ACOs.
Finally, within ACOs that had lower savings, we identified fewer with downside risk models. This could be correlated to an ACOs maturity in the program: ACOs that continue to participate year over year may gradually take on more risk as they refine their strategy. This is important in context of the new Pathways to Success program, as it shortens the length of time required for ACOs taking on risk from six years to two (high revenue) and three (low revenue) year.3
In our initial analysis, we were not able to identify associated trends by track type, quality score, patient Medicare cohorts or avg HCC risk score. However, this led us to dig a bit deeper into other areas that may influence success in MSSP, specifically cost and utilization of services.
Profiling ACO Success: Which expenditure categories contribute to high or low spend?
At a high level, we see that top performing ACOs on average spend 10% less per beneficiary than those who lost savings – this accounts for over $1,200 in spend per member per year (PMPY) in PY 2019. This trend remains consistent over the last three years of performance, 2017 – 2019. The top performing quintile not only continues to spend less overall, but we see similar trends in how spend is distributed across the Medicare expenditure categories: Part B, and Part A (inpatient, outpatient, home health, skilled nursing and hospice facilities).
Key Findings
- ACOs in the top quintiles by savings per capita contributed lower expenditures across all Part A services
- Within Part A, Outpatient and Skilled Nursing Facility (SNF) services have the largest difference in spend across ACO quintiles
- Top performing ACOs (top 20% of highest savings per capita) spend less in every category except Part B; and in fact, they spend ~7% higher in Part B than any other ACO quintiles
Within Part A, it’s no surprise we observe ACOs with the most savings are spending less across facility services as seen in the table below. ACOs can play an important role when coordinating the right care in facility settings, and have shown to reduce overall facility expenditures in a given population.4 The greatest difference in spending from ACOs in the top quintile compared to their peers was at the SNF and outpatient setting; boasting an average of over 30% lower cost than those that did not make savings.
Within the SNF setting, ACOs set a precedent for their focus on coordinating high quality and low cost care, and is highlighted by CMS as a key strategy for success in value based care programs.5 As shown in the table below, ACOs in top quintiles have significantly lower SNF PMPY than those who did not make savings. This could be indicative of some active care coordination in transitions to post acute care. Additionally, we see a slight increase in Home Health utilization among the top cohorts, which could signal re-routing patients, where appropriate, to the home setting. Not only is home health usually less expensive, but it is often just as effective as caring for a patient in a hospital or SNF.6 This CareJourney analysis expands on trends in home health utilization, and what the future of home health may look like in a post-pandemic world.
| 2019 MSSP Performance Results: Expenditures by ACO Quintile per Member per Year | ||||||||
|---|---|---|---|---|---|---|---|---|
| Part A | ||||||||
| ACOs Ranked by Total Savings per capita | Total Risk Adjusted | Total PMPY | Part B | Inpatient | Outpatient | SNF | Home Health | Hospice |
| Top 20% | 11,567 | 11,976 | 3,998 | 4,025 | 2,174 | 681 | 571 | 251 |
 |
11,460 | 11,208 | 3,408 | 3,775 | 2,344 | 616 | 546 | 248 |
| 11,738 | 11,565 | 3,365 | 3,854 | 2,574 | 705 | 521 | 265 | |
| 11,804 | 11,823 | 3,378 | 3,981 | 2,669 | 692 | 538 | 275 | |
| Bottom 20% | 12,762 | 13,249 | 3,714 | 4,601 | 2,879 | 889 | 603 | 283 |
Figure 4: CareJourney 2019 MSSP Performance Results Analysis: ACOs Quintiled by Total Savings per Beneficiary, total expenditures by category
We also observed that outpatient spend decreases across ACOs with more generated savings – accounting for over $700 PMPY between the top and lowest ACO quintiles. Since this category only includes expenditures billed in a facility setting, one explanation could be strategic efforts to increase utilization of outpatient services in Part B that are lower cost; ACOs in the Top 20% spent 8% more in Part B vs. the Bottom 20%. For example, Ambulatory surgery centers (ASCs) are modern healthcare facilities billed under Part B that provide same-day surgical care, including diagnostic and preventive procedures, and claim to deliver lower cost and more efficient services than outpatient hospital departments.7 Finding opportunities to switch the site of service, where appropriate, could be an important strategy for any VBC organization to leverage. While site of service switching opportunities from Part A facilities could be redistributing costs to Part B, we wanted to dig deeper into overall utilization of all services.
Profiling ACO Success: What types of services are being utilized?
In addition to expenditures, utilization of services is just as important for ACOs to help ensure patients are getting the right care at the right time. We conducted a brief, high level analysis to evaluate utilization of services and give context on the expenditure trends outlined above. Consistent with increased Part B spend, we saw significant utilization of PCP related visits.
Key Findings
- ACOs in the top quintile by savings per capita have the highest utilization of Evaluation and Management (E&M) services
- ACOs in the lowest quintile by savings per capita have the highest utilization of SNF, Emergency Department (ED) & Inpatient (IP) admissions
As seen in the table below, ACOs in the top quintile have the highest utilization of E&M services, a 7% increase over all other quintiles. Primary care physicians are at the core of ACO management – they help manage chronic diseases, foster patient health engagement, and coordinate services through taking a proactive approach to their patient’s care. In turn, this can impact spend and utilization of higher cost services downstream.8 This is similar to what’s profiled in our expenditure data for ACOs in the highest quintile: higher Part B costs with lower cost facility services.
| 2019 MSSP Performance Results: Utilization per 1,000 Beneficiaries by ACO Quintile | ||||||
|---|---|---|---|---|---|---|
| ACOs Ranked by Total Savings per capita | SNF Admits per 1k | HHA Visits per 1k | PCP Visits per 1k | IP Admits per 1k | ED Visits per 1k | Avg Readmission Rate |
| Top 20% | 76 | 3,590 | 12,454 | 303 | 656 | 19% |
 |
73 | 3,448 | 11,018 | 286 | 678 | 18% |
| 74 | 3,385 | 10,812 | 287 | 657 | 18% | |
| 76 | 3,448 | 10,911 | 292 | 690 | 18% | |
| Bottom 20% | 87 | 3,730 | 11,777 | 311 | 713 | 19% |
Figure 5: CareJourney 2019 MSSP Performance Results Analysis: ACOs Quintiled by Total Savings per Beneficiary, utilization by category
ACOs who generated net positive savings overall, had lower numbers of Inpatient admissions and Emergency room visits than those who did not generate savings, but there doesn’t appear to be any correlation with quintile, or overall magnitude of savings. Similarly to the acute setting, SNF utilization remains nominally consistent within ACOs that made savings, but ACOs that did not make savings clearly standout from their peers with higher SNF admits. There is higher utilization of Home Health in the top cohort compared to their peers. In the context of our expenditure analysis, this could highlight the importance of not just reducing utilization of unnecessary services, but finding the right opportunities for coordination and intervention.
Profiling ACO Success: Are Care Management services being leveraged?
The next step of our analysis included how ACOs leverage specific visits types in primary care: Annual Wellness Visits, Flu Shots, Transitional Care Management, and Advanced Care Planning. These care management services were created to enable primary care practices to help patients stay healthy and out of the hospital by spending more time focused on prevention and wellness.9 We’ll explore these visit types in context of our top ACO performers quintile below.
Key Findings
- AWV compliance rate increased by 10% across the the ACO quintiles
- ACP compliance nearly doubled for those in the top ACO quintile, though continues to remain underutilized overall
- Flu shot and TCM have nominal changes in compliance across the ACO quintiles
Most notably, Annual Wellness Visit (AWV) compliance increased by 10% across the ACO quintiles; meaning these top performing ACOs were able to engage, on average, roughly 1,400 more patients through AWVs that year compared to their peers. Facilitating change in healthcare can often feel like trying to steer a cruise ship: large amounts of effort for what seems like a few degrees of change. However, when we think about the potential to fundamentally change 1,400 patients’ healthcare experiences, these initiatives become invaluable. There also may be care management strategies for ACOs to implement that allow the greatest impact. For example, a study conducted by Aledade found that patients who received their first AWV experienced a meaningful reduction in adjusted total healthcare costs of 5.7 percent, with the greatest association seen for the highest risk patients.9 While there are a lot of factors to consider when measuring the clinical efficacy of these visit types, it is uplifting to see that ACOs who generate high savings can be correlated with preventative care initiatives.
| 2019 MSSP Performance Results: Care Models by ACO Quintile | ||||
|---|---|---|---|---|
| ACOs Ranked by Total Savings per Capita | Avg AWV Compliance Rate | Avg Flu Shot Compliance Rate | Avg TCM Compliance Rate | Avg ACP Compliance Rate |
| Top 20% | 47% | 54% | 24% | 11% |
 |
43% | 55% | 23% | 8% |
| 38% | 53% | 19% | 6% | |
| 38% | 54% | 22% | 5% | |
| Bottom 20% | 37% | 51% | 20% | 6% |
Figure 6
Other less well-known visit types include Transitional Care Management (TCM) and Advanced Care Planning (ACP). TCM is intended for primary care physicians to help facilitate the hand-off period following an inpatient, SNF or other facility stay to a home or community setting. TCM visits can help prevent unnecessary readmissions and potentially reduce costs by ensuring a smooth transition of care.10 Through our data, we can see that ACOs with top savings had slightly higher rates of TCM compliance, but no significant trends were identified.
Conversely, ACP compliance nearly doubled for ACOs in the top quintile. ACP services are used to discuss the patient’s health care wishes (e.g. Advanced Directives) if they become unable to make decisions about their care in the future. ACPs can help coordinate the appropriate care and symptom relief while reducing costs.11 As shown in the data above, ACOs with higher savings are more frequently leveraging ACP visits; however, it is generally underutilized across ACOs and the industry overall.12 This could be an example of where the ‘degree of change’ seems nominal for an ACO’s strategy, but is a part of multiple initiatives for overall success.
See over 200+ cost, utilization, and quality metrics paired with total and per capita generated savings.
Explore with CareJourney
This analysis gives us one lens to view ACO performance, but as demonstrated in the data, there is no perfect answer for success in MSSP. It is rather more of a huge coordinated effort of initiatives across the entire patient journey. In practice, we can see that there are trends across ACOs that earn high caliber savings, specifically a strong focus of Part B services as a method for preventive care, coordination, and reducing costs downstream.
But, there is more still to discover about what creates success in MSSP, such as:
- Understanding how an ACO’s patient population demographics & geography impacts their strategy
- Year over Year trend analysis
- Deep dive on Post Acute care and Part B services
- Evaluating the strength of care management services
In the meantime, there are several ways in which CareJourney can further support value based organizations to take these insights and drive actionable next steps, including:
- Evaluate the potential savings in switching the site of service for procedures, imaging & labs for an attributed population
- Track care management compliance from all levels of an organization: patient, provider and group levels
- Understand utilization of services from an attributed population and cultivate strong preferred provider & facility networks
- Leverage CareJourney claims ingestion and transformation Population Insights tool to track care interventions in real time
If you are currently a member and interested in how CareJourney can help you gain insights into designing and managing a value based organization, please reach out to your Member Services representative for more information. If you are not a CareJourney member, please email us at jumpstart@carejourney.com, or you can learn more by requesting a meeting below.
-
About the Program | CMS. (n.d.). CMS. Retrieved April 1, 2021, from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/about
-
CMS Finalizes “Pathways to Success,” an Overhaul of Medicare’s National ACO Program | CMS. (2018, December 21). CMS. https://www.cms.gov/newsroom/press-releases/cms-finalizes-pathways-success-overhaul-medicares-national-aco-program
-
ACO Care Coordination Tool Kit. (2019, March). CMS. https://innovation.cms.gov/files/x/aco-carecoordination-toolkit.pdf
-
Medicare Program Shared Savings Accountable Care Organizations Have Shown Potential For Reducing Spending And Improving Quality. (2017, August). Department of Health and Human Services. https://oig.hhs.gov/oei/reports/oei-02-15-00450.pdf
-
Medicare Home Heath Beneficiaries. (2021, April 26). CareJourney. https://carejourney.com/medicare-home-health-beneficiaries/
-
Study: Medicare Cost Savings Tied to ASCs – Advancing Surgical Care. (n.d.). Higher Logic, LLC. Retrieved April 1, 2021, from https://www.advancingsurgicalcare.com/reducinghealthcarecosts/costsavings/medicarecostsavingstiedtoascs#:%7E:text=Because%20Medicare%20reimburses%20ASCs%20at,ASC%20instead%20of%20a%20hospital
-
Paying More for Primary Care: Can It Help Bend the Medicare Cost Curve? (2012, March). Commonwealth Fund. https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_issue_brief_2012_mar_1585_reschovsky_paying_more_for_primary_care_finalv2.pdf
-
New Study: In Physician-Led Accountable Care Organizations Medicare Annual Wellness Visits Are Assoc. (2020, December 11). Aedade. https://resources.aledade.com/press-releases/new-study-in-physician-led-accountable-care-organizations-medicare-annual-wellness-visits-are-associated-with-improved-health-care-quality
-
Ballard, J. (2018). Effect of Ambulatory Transitional Care Management on 30-Day Readmission Rates. PubMed. https://pubmed.ncbi.nlm.nih.gov/29745236
-
Advance Care Planning in an Accountable Care Organization Is Associated with Increased Advanced Directive Documentation and Decreased Costs. (2018, April 1). PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5867515
-
Skolarus, L. E. (2021, November 1). Regional Variation in Billed Advance Care Planning Visits. PubMed. https://pubmed.ncbi.nlm.nih.gov/32805062
