Background
To date, 48 states plus the District of Columbia have implemented value-based care initiatives in one form or another. Driven by both efficiency and outcome, value-based care (VBC) models rely heavily on healthcare data from payors, providers, and patients in order to optimize performance. As more healthcare systems accept VBC models as the way of the future, they must become experts in handling real-world healthcare data to optimize their own operations.
Here’s a look at what VBCs do with healthcare data and how they improve outcomes as a result:
1. Link Funding and Patient Outcomes
VBCs use data regarding healthcare outcomes to determine payments, thereby incentivizing positive outcomes, innovation, and improvement. Though performance-based funding adjustments are typically made in small increments, even a small variation is significant to a multi-million-dollar healthcare system.
VBC models now fund more than 1/3 of all healthcare payments. The average hospital revenue in the US is over $190 million. Because of this volume, even a small percentage decrease under a VBC model can result in large savings opportunities.
Incentivizing positive patient outcomes allows VBCs to promote the best and most efficient care for their constituents.
Provider Rankings By Positive Outcome
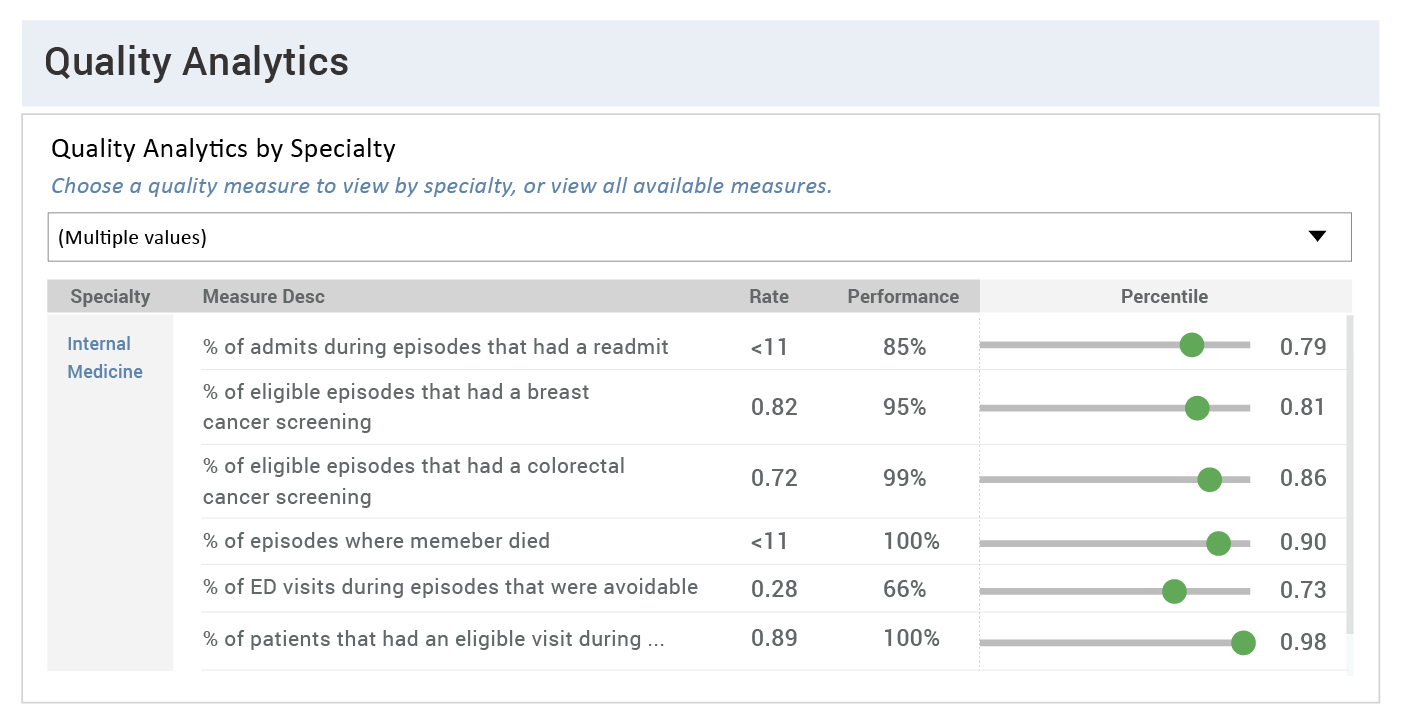
Data Source: CareJourney
In the example above, a VBC provider practice can identify where providers are out-performing their peers in a particular area of care, such as the number of patients who receive their annual wellness exams and screenings. They can then investigate what’s driving the improvement, and incentivize other providers to implement these practices.
2. Generate Peer-to-Peer Comparisons for Provider Evaluation and Benchmarking
Provider comparisons create a baseline from which VBCs can monitor changes in performance, in order to reward improvement or bring attention to negative trends. Healthcare isn’t a competition, but it is valuable for medical providers, hospitals, and healthcare systems to understand how they compare to their local and national peers.
Provider Rankings in a Single CBSA Based On Effectiveness
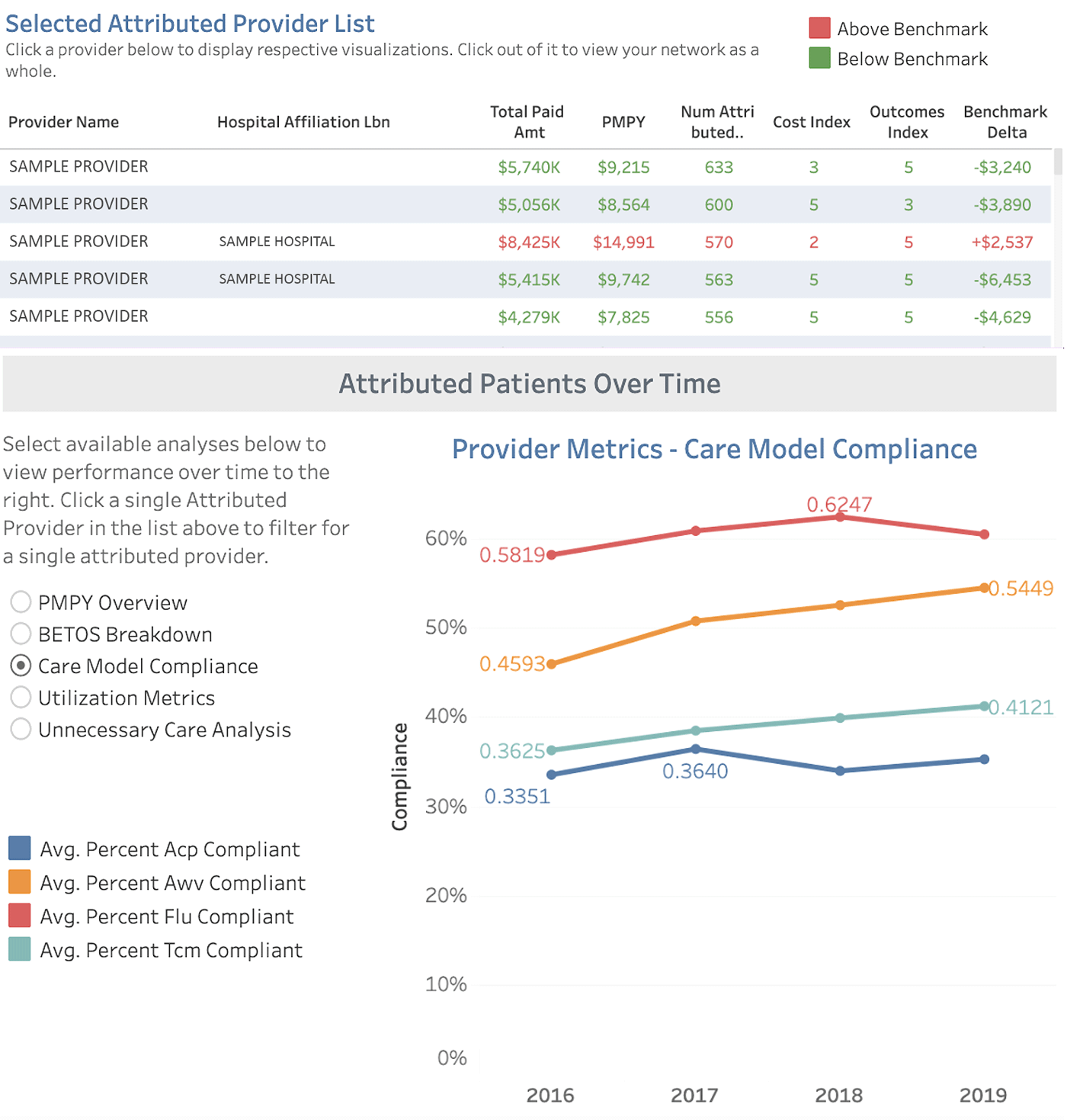
Data Source: CareJourney
Patient outcomes are paramount, and if a practice is delivering a lower quality of care, opportunities for its growth are limited. In healthcare, data-driven benchmarking has an increasing impact on both improved patient outcomes and long-term growth for practices, hospitals, and systems.
Provider metrics that matter include:
- Patient satisfaction scores
- Long-term patient outcomes
- Quantity of tests ordered as compared to similar providers
- Percentage of patients who comply with annual screenings and exams
3. Reward Efficiency in Operations & Outcomes
In order to deliver more efficient healthcare with better outcomes for patients and lower costs for insurers, data factors like the length of time from intake to release and the length of treatment required are incorporated into VBC models. VBCs aim to move patients quickly through acute situations and into stable health without delays or barriers to care.
Providers Ranked By Efficiency Factors/Faster Recoveries
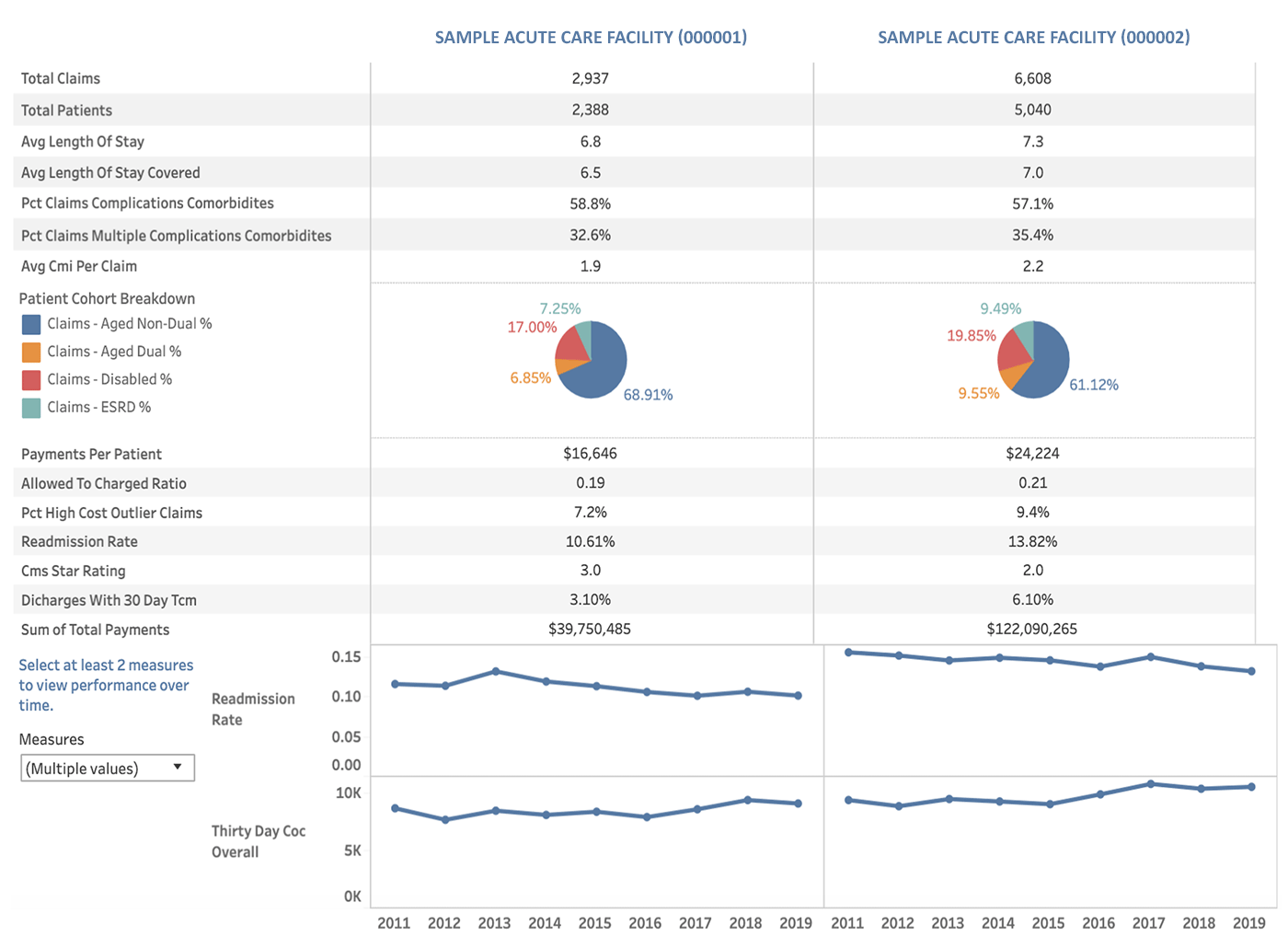
Data Source: CareJourney
Healthcare data can be used to illustrate where providers are encountering challenges or delays so that the root of the problem can be identified and eliminated. For example, a hospital administrator might look at how the hospital’s doctors are ranked for the following metrics:
- Average time between intake to release
- “Frequent flyer” patients who get released only to be admitted again
- Duration of outpatient treatments like chemotherapy, dialysis, or physical therapy
4. Focus on Coordinated Care Performance
Patient outcomes improve when their providers work together to deliver the services they need. VBCs use coordinated care data scores to evaluate how well a patient’s providers are communicating and executing on necessary services. Delays in care, extended delivery, and patient dissatisfaction are all factors in the review of coordinated care teams.
In Network vs CBSA Care Model Compliance
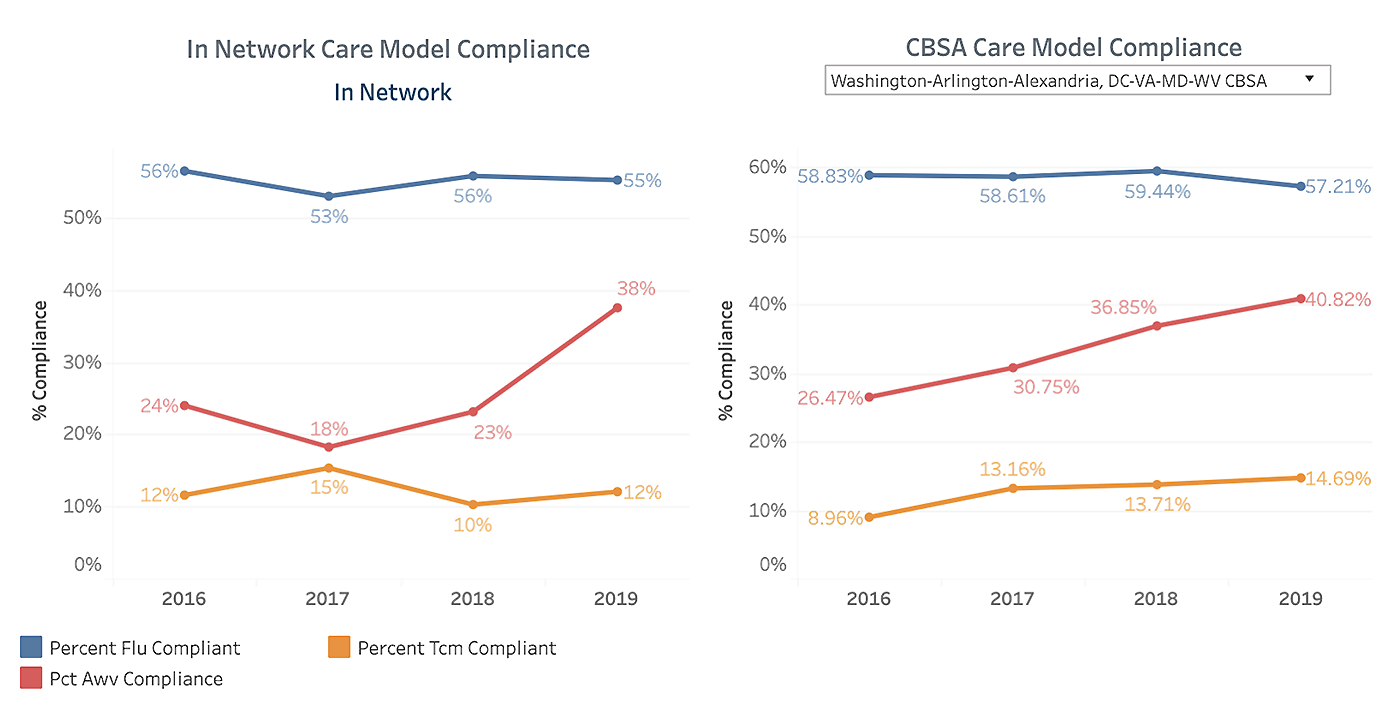
Data Source: CareJourney
Referrals, appointment setting, inadequate tracking of test results and other factors all reduce the effectiveness of coordinated care and limit growth potential for healthcare systems. In fact, a 10% improvement in system referral retention is equivalent to a 10% growth in volume – significant for any medical practice. Examining the following data points can allow administrators to identify and resolve continuity of care issues:
- Number of repeat tests due to lack of continuity
- Days elapsed between the time of a referral until the patient had an appointment
- Percentage of patients that did not follow through on post-acute care
5. Monitor Local, Regional, and National Data
Under the VBC model, states tend to be the definitive marker for peer-to-peer comparisons. However, both larger and smaller data sets are also monitored to determine factors that may impact access to and outcomes of critical care.
Data Comparison Between States or Regions
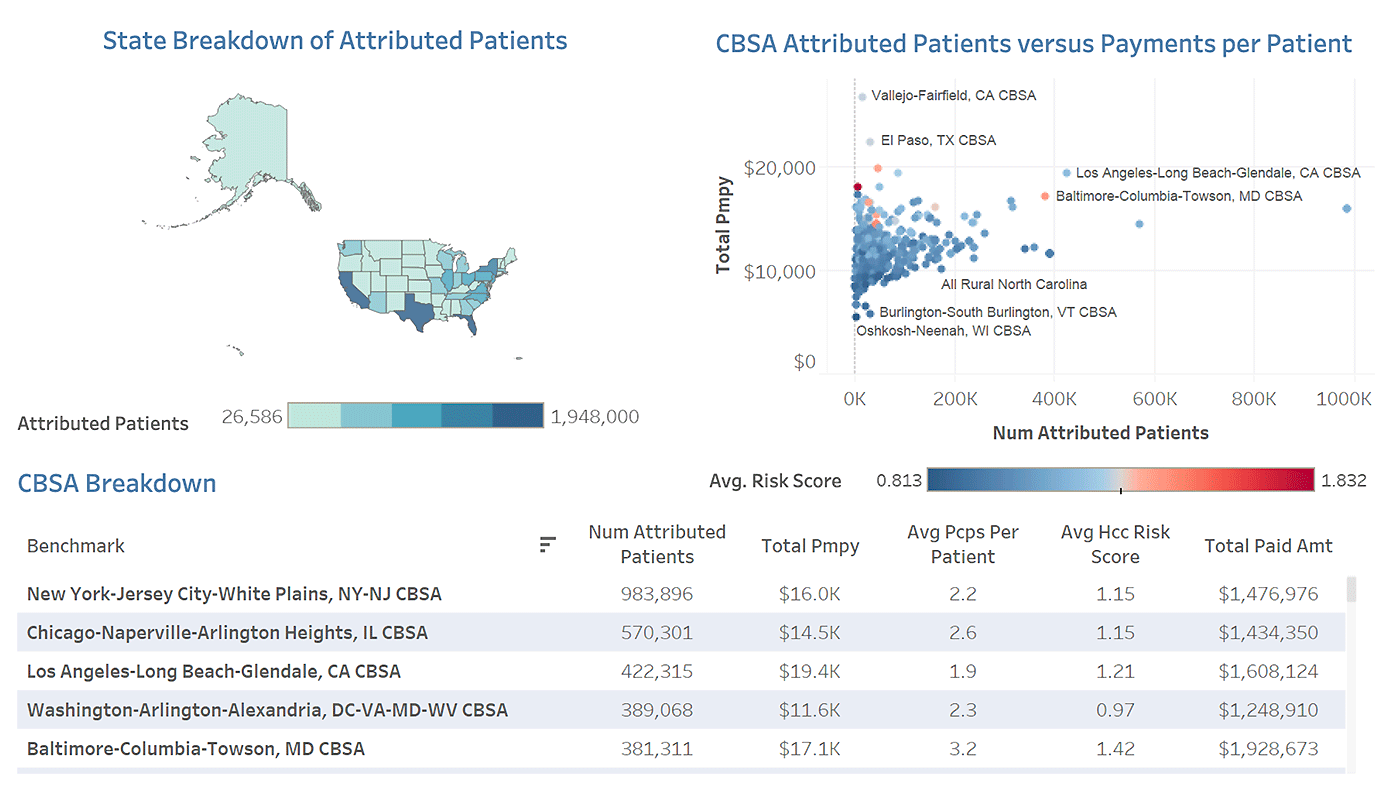
Data Source: CareJourney
By tracking local, regional, and national healthcare data, VBCs identify areas of success that can serve as models to improve areas of concern. In addition, regional comparisons allow healthcare systems to understand and address the socioeconomic factors that create barriers to care for many constituents. Breaking healthcare data down by demographics including race, sex, and income, as well as comparing urban and rural or city and suburban locations is an effective way to understand the different factors that drive healthcare behaviors in a given area.
The VBC model is becoming a standard for healthcare organizations. Learn more about how CareJourney, the #1 Provider of Value-based Care Analytics, can help your organization make the best use of data in improving patient outcomes and delivering quality care that attracts new patients. Request your demo today.
