Two Unwanted Players in Value-based Care: Fraud and Waste
How ACOs Can Mitigate Their Exposure
By Erica Everhart and Zach Bredl
September 18, 2024
Inherent in their design, Accountable Care Organizations (ACOs) are responsible for the total care of their assigned patient population. Their savings are based on the overall quality, quantity, and cost of care their beneficiaries receive. This alone is no easy feat. Yet, for those ACOs participating in Centers for Medicare and Medicaid Services (CMS) programs, there is an added complexity that commercial ACOs do not face.
Within these CMS programs, ACOs cannot mandate beneficiaries seek care only from affiliated providers. In addition, these ACOs cannot utilize prior authorization to deny care (for example, new expensive treatments without demonstrated outcomes). This leaves ACOs particularly vulnerable to wasteful spending or bad actors perpetuating fraudulent spending.
As described in recent headlines, these ACOs stand by watching the impacts of fraud or waste across their population with no recourse. Any potential relief comes in the form of legislative rulemaking or CMS policies, both of which take time to create and work their way through the approval process. They also do not provide guaranteed relief of this spend, particularly if it is not fraudulent and “simply” wasteful.
In the post below, we highlight the data behind these headlining fraud and waste stories, as well as ways ACOs can mitigate impacts.
2023’s Fraud Headline: Urinary Catheters
In 2023, a Medicare fraud scheme made mainstream news, costing the government an estimated $2B. Under this scheme, fraudulent actors preyed on Medicare beneficiaries through phone calls and other forms of contact offering them “free services” and enrolling these beneficiaries in monthly Medicare billing for urinary catheters. Yet, beneficiaries did not receive these catheters.
To contextualize this, the table below shows 2023’s top billing codes by dollar value in Traditional Medicare (excluding Medicare Advantage). Across the list, urinary catheter spend jumps out as the highest amount paid with over $2.6B (billing code A4353). This was one of the two billing codes involved in the catheter fraud. While not all of this spend was fraud, billing for this same code only amounted to $43M in 2022 (the year prior).
Top 9 Billing Codes by Total Paid, Traditional Medicare, 2023
**This excludes office visits, hospital visits, etc. (codes: 99214, 99213, 99232, 99233, 99215, 99204, 99223, 97110, A0427, 99285)
| Billing Code | Description | Total Paid – 2023 |
|---|---|---|
| A4353 | Intermittent Urinary Catheter | $2,698,595,823 |
| J0178 | Eylea Injection (AMD Treatment) | $2,360,684,141 |
| K1034 | Provision of Covid Test | $1,828,539,619 |
| 66984 | Cataract Removal With Insertion Of Intraocular Lens Prosthesis | $1,575,322,675 |
| J9271 | Keytruda Injection (Immunotherapy for Cancer) | $1,522,011,289 |
| Q4262 | Dual layer Impax Membrane, per square centimeter | $1,109,708,922 |
| G0439 | Annual Wellness Visit | $1,070,860,788 |
| J2777 | Vabysmo Injection (AMD treatment) | $990,228,268 |
| A4239 | Continuous Glucose Monitor | $937,686,689 |
While the sheer paid amount for these catheters shows the detrimental impact to the US healthcare system, it is a particularly acute problem for ACOs. Under traditional CMS financial reconciliation, savings or loss calculations for ACOs would have included the costs of the catheters. The inclusion of fraudulent amounts could be the difference between attaining savings or paying losses for many ACOs – the bedrock to fund their programs for subsequent years.
With this in mind, on June 28, 2024 CMS issued a proposed rule to remove all catheter spend for two billing codes from savings calculations for Medicare Shared Savings Program (MSSP) ACOs and Realizing Equity, Access, and Community Health (ACO REACH) ACOs for 2023. Further, in the recently released Physician Fee Schedule, CMS also proposed a process for handling fraud for MSSP ACOs in future years. Financial reconciliations for ACOS for Performance Year 2023 have been delayed by six weeks due to these necessary changes.
While these policies are helpful, they are defensive, leaving ACOs in limbo and at the mercy of legislatures while observing these trends in real time.
2024’s Fraud Headlines: Wound Grafts
Continuing the fraud headlines, in June 2024, the Department of Justice announced indictments of 193 defendants committing another $2.3 billion dollars in fraud – outside of the 2023 fraudulently billed urinary catheters. Among these defendants, four were indicted for over $900M in Medicare fraud involving amniotic wound grafts. These grafts are frequently used with diabetic ulcers or venous ulcers patients. The defendants are charged with unnecessarily treating superficial wound patients, and further treating them with grafts far larger than necessary (An important consideration – these grafts are billed by the square centimeter).
In reviewing 2023’s top codes billed again (table above), Dual Layer Impax Membrane (billing code Q4262) stands out with over $1.1B in total paid amounts. Dual Layer Impax Membrane is an amniotic wound graft typically used to treat diabetic foot ulcers and venous ulcers. It is no surprise that the first five providers billing these codes in 2023 (table below) are affiliated with APX Mobile (part of the DOJ’s indictment) and two of those five providers are facing criminal prosecution.
Top 10 Providers Billing Dual-Layer Impax Membrane by Amount Paid, Traditional Medicare, 2023
| Provider Name | State | Amount Paid | Criminal Status |
|---|---|---|---|
| REDACTED | Arizona | $135,160,596 | Affiliated with APX Mobile (Not charged by DOJ) |
| REDACTED | Arizona | $123,792,249 | Affiliated with APX Mobile (Not charged by DOJ) |
| REDACTED | Arizona | $83,663,242 | Affiliated with APX Mobile (Not charged by DOJ) |
| Carlos Ching | Arizona | $62,886,995 | Affiliated with APX Mobile (Charged by DOJ) |
| Bethany Jameson | Arizona | $42,318,310 | Affiliated with APX Mobile (Charged by DOJ) |
| REDACTED | Arizona | $27,010,659 | None |
| REDACTED | Arizona | $23,271,013 | None |
| REDACTED | Nevada | $23,167,658 | None |
| REDACTED | Colorado | $20,659,651 | None |
| REDACTED | Arizona | $16,838,664 | None |
While this one group heavily influenced the overall Dual-Layer Impax Membrane spend in 2023, it does not account for all of it. It is important to note that not all the spend is fraudulent; however, there is still over $600M spent by other providers on this one billing code grabbing it a spot in the top 30 most expensive billing codes of 2023.
For ACOs, this has the same effect as the catheter spend, but in a completely different practice area – rising spending trends without the ability to mitigate through prior authorization or narrow networks.
A Parallel Story of Waste
To attribute all this rising spend as fraud is inaccurate. However, there is an undeniable increase year over year and another culprit is likely waste.
To contextualize further, the chart below looks at all skin substitute and wound graft billing codes more broadly – not just Dual Layer Impax Membrane. The skin substitute market saw multiple new-entrants in 2023, many of which are high cost. The chart below shows that ACOs on average spent over twice as much per beneficiary on skin substitutes in 2023 than in 2022, but saw a less steep increase than for beneficiaries not enrolled in ACOs.
The Rapid Growth of Skin Substitute Billing
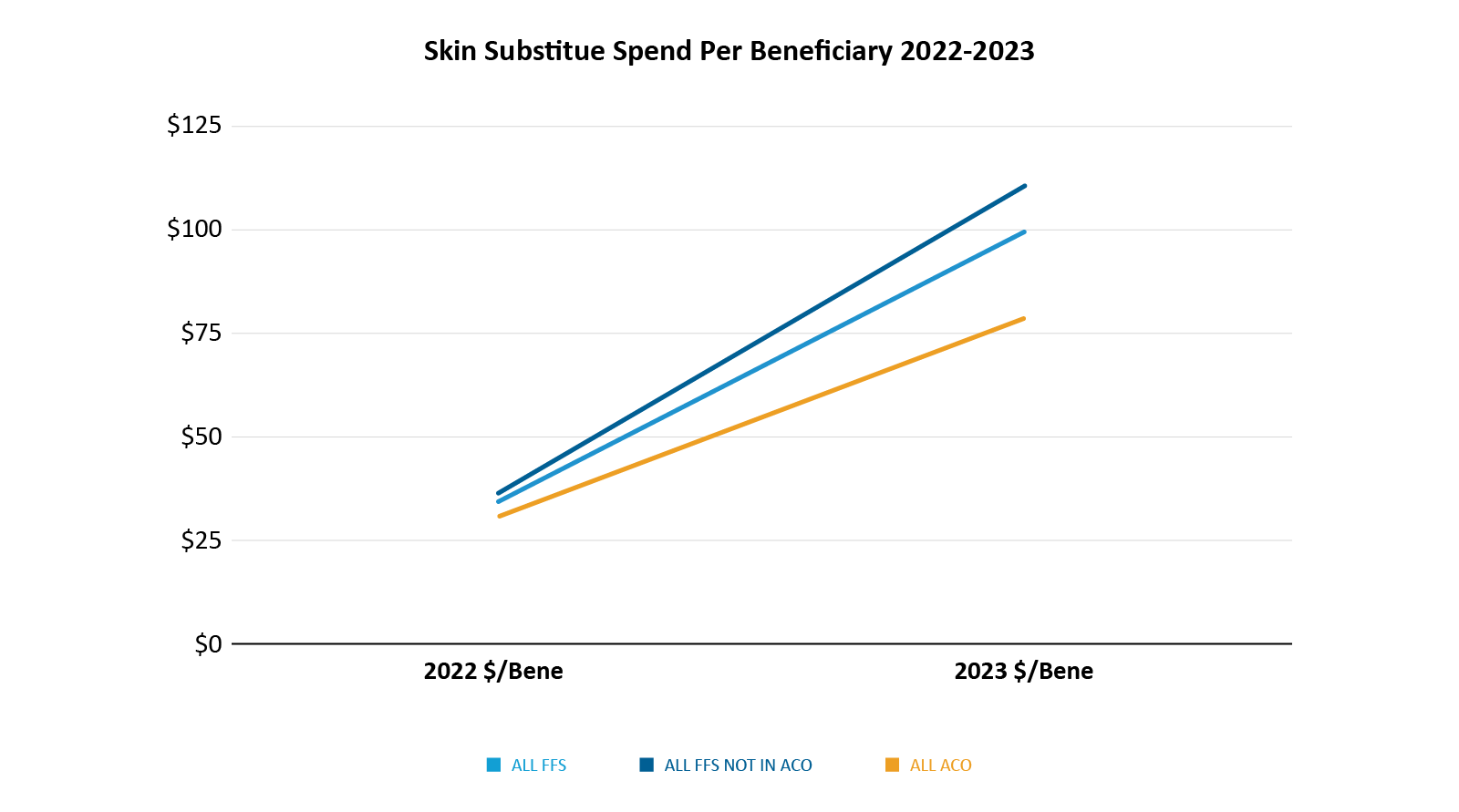
In the MSSP and ACO REACH charts below, the rise in spend for skin substitutes from 2022 to 2023 by ACO is evident. Interestingly, the ACOs with the highest per beneficiary spend on these skin grafts were not impacted by the providers indicted by the DOJ.
This suggests waste.
In programs like MSSP and REACH where savings are made or lost on thin margins, an average $200 to over $1000 average increase in per member per year costs could be devastating.
2022-2023 Skin Substitute Growth by Top ACO REACH and MSSP ACOs
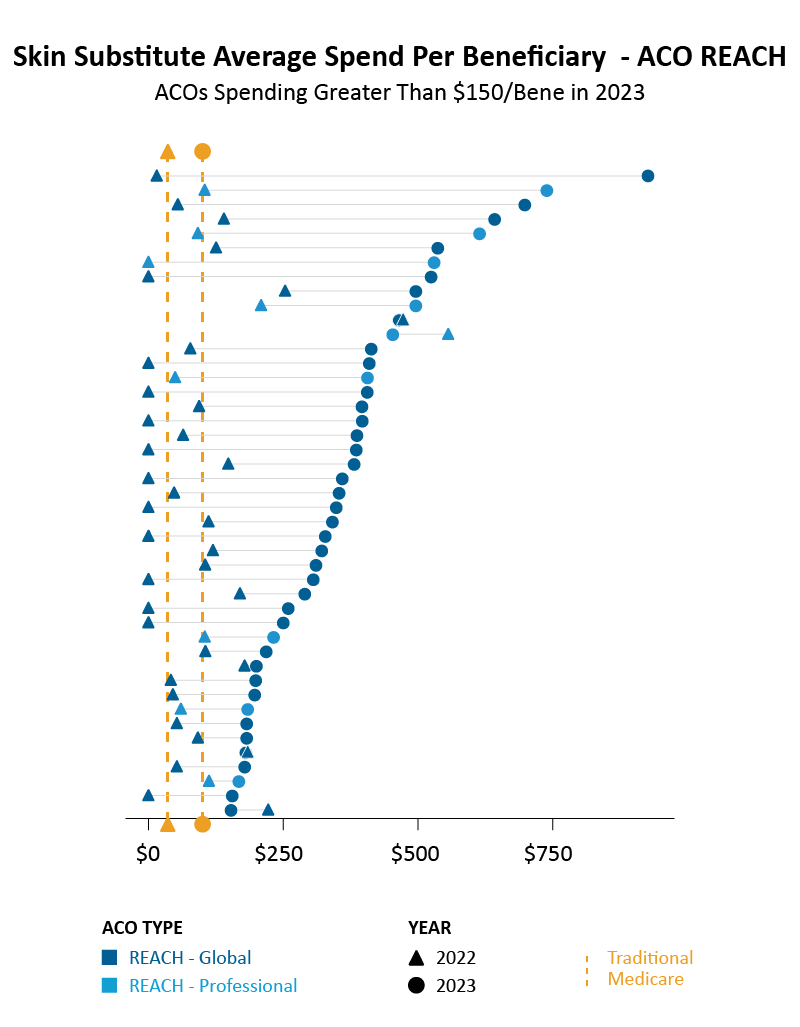
Each line above represents a unique ACO.
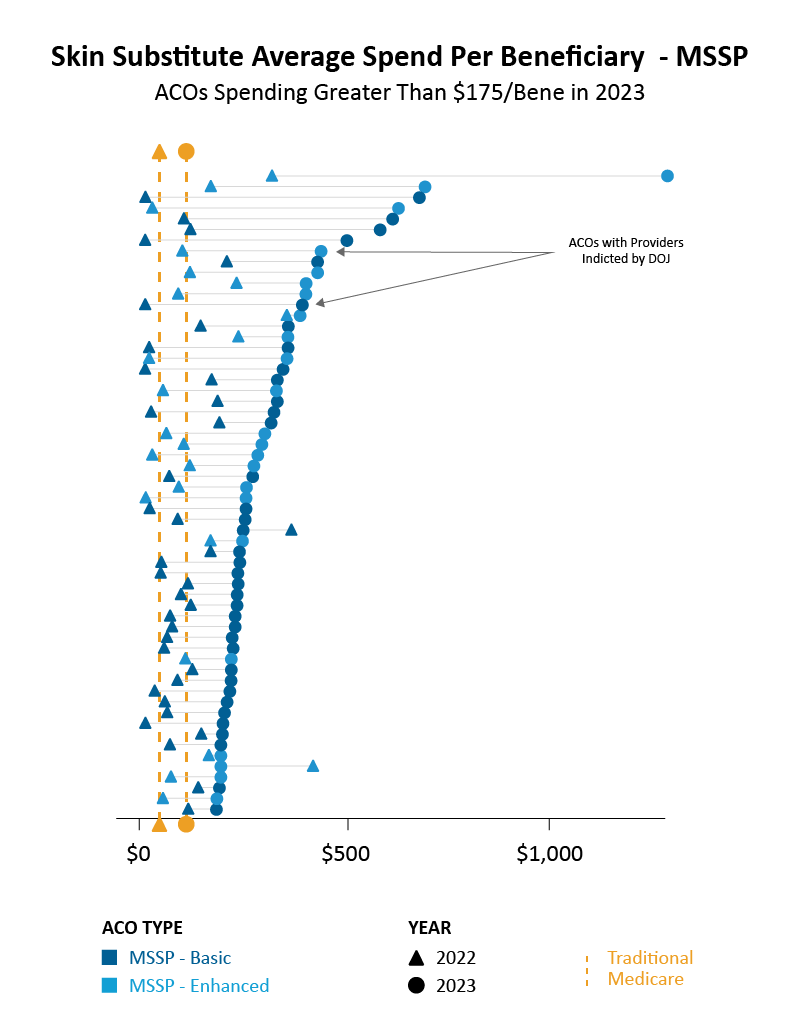
Each line above represents a unique ACO.
Mitigating Exposure
Seeing dramatic increases in spend like these is concerning for any ACO – especially if they aren’t seeing it until too late. So, what is an ACO to do? What steps help ensure spend is appropriate and mitigate waste?
There are two in particular that we recommend:
Build a Claims Monitoring System
ACOs receive claims data from CMS either in the form of monthly claims files or the timely Beneficiary Claims Data API (BCDA). With this data as a foundation, ACOs should build a claims monitoring system observing volumes of claims by site of service, region, practice group, BETOS category (used for the analysis above), and more.
After identifying rising trends across a category, it is necessary to dive further into billing codes to unpack the drivers of the spend. For example, Dual-Layer Impax Membrane, the top most expensive skin substitute for 2023, is part of the problem with increased spend, but it is not the full problem. In fact, five different billing codes accounted for 61% of the national Traditional Medicare spend for skin substitutes, with each individually accounting for more than 5%. To focus only on Dual-Layer Impax Membrane wouldn’t have fully solved the problem.
Within claims monitoring, ACOs should also monitor on a provider level. Specifically, we recommend provider level reporting for:
- New providers billing to your ACO
- Significant billing in terms of claims and dollars
- Out-of-state billing
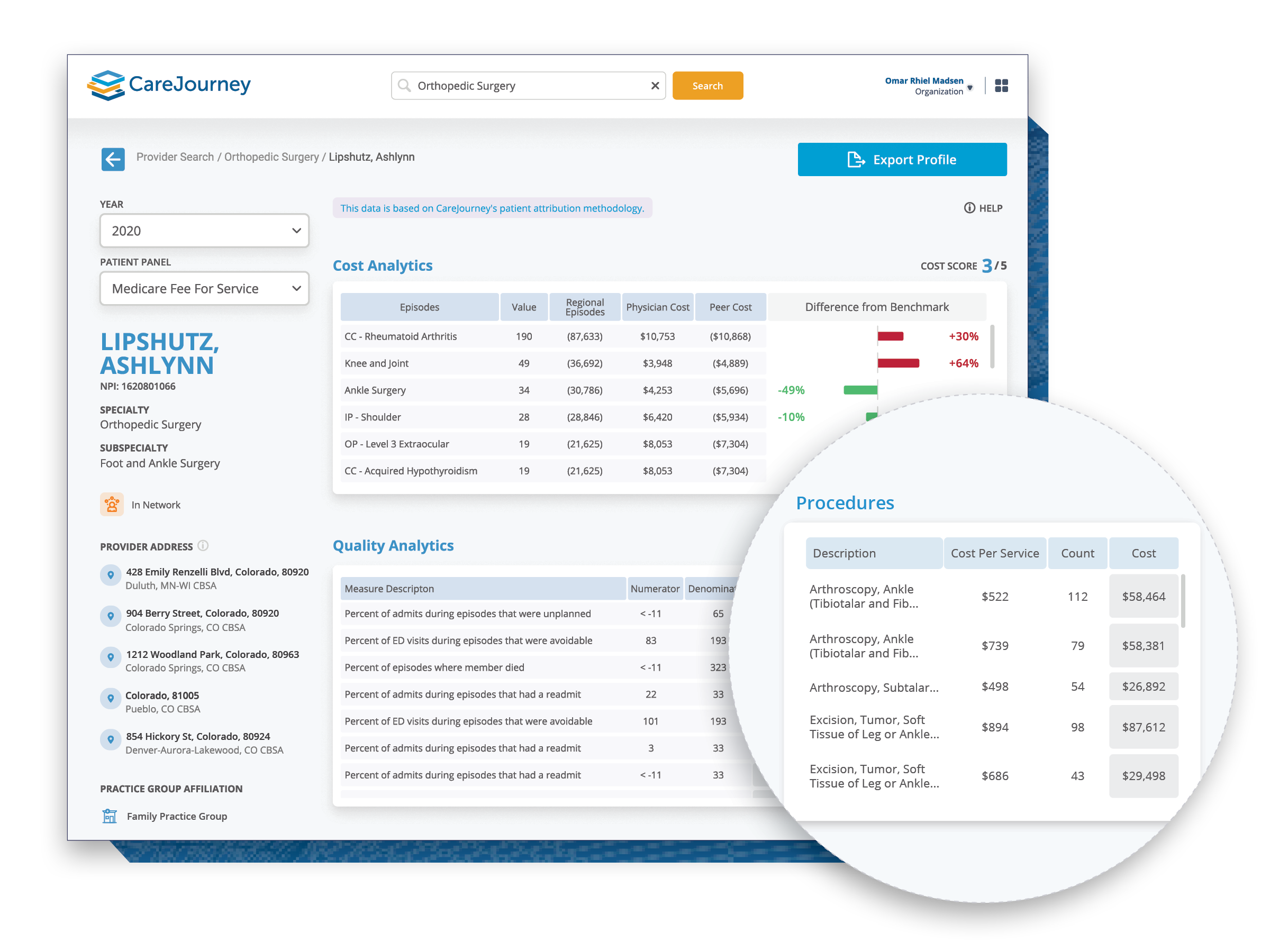
To maximize impact with claims monitoring, organizations should use BCDA data to identify high billing (and potentially fraudulent) providers weeks, or even months, before any other data. The dashboard below shows a sample snapshot of how CareJourney helps organizations surface and analytically enrich these insights from their raw data.

Create Meaningful Incentives
A second tactic to mitigate risk for fraud and waste centers around shared risk – the most powerful way an ACO can increase high value care for beneficiaries. Specifically, ACOs can enlist providers (particularly specialists given their higher spend) to share in the patient risk via bundled payments or other risk-shifting arrangements..
In the skin substitute example, a vast majority of providers are still operating under a pure fee for service system. The doctors prescribing Dual-Layer Impax Membrane, a newcomer to the market in 2023, are likely doing so because they believe it a better product, but without evaluating the cost of the product. Under a bundled payment system, an ACO would create an agreement with wound care specialists allotting a flat rate (bundled payment) to treat diabetic foot ulcers. This pushes providers to consider the relative value of the Dual-Layer Impax Membrane alongside the cost of the product – ensuring value and appropriate usage. The ACO can ensure high quality care by withholding a portion of the bundled payment contingent upon satisfactory quality measured by a pre-selected set of measures.
Episode groupers, such as the Episode Grouper for Medicare, allow for the creation of these bundles by ACOs. For example, the Medicare episode for skin graft surgery on a diabetic foot ulcer establishes a 12-week episode in which physicians are accountable for the procedure, as well as subsequent follow up. ACOs can analyze the historical, risk adjusted costs for the episode, including related complications such as emergency room visits, readmissions, re-application of the graft, and infections over those twelve weeks to set a bundle price that incentivizes high quality care without compromising provider discretion.
ACOs are only able to create these bundles with sufficient data – Data to create the bundles, data to model out performance scenarios, data to track transparent quality measures, and data to understand performance live.
Support Your Strategy
There is no doubt that fraud and waste have become an increasingly present concern for ACOs. The impacts can have huge ramifications on organizations, their shared savings, patients, and the value based care system overall.
Having the right data partner to help enrich and take action on your earliest data indicators, as well as benchmark trends across the complete historical picture, helps reduce the burden and allows focus on what matters most – delivering high quality care. Our analytics, product suite, and services team are here to help.
About CareJourney by Arcadia
CareJourney was founded in 2014 under the belief that our nation’s transition to value-based care is an important one, but without an “operating manual” that can reliably deliver on the promise of better quality at a lower cost. Our mission is to empower individuals and organizations they trust with open, clinically-relevant analytics and insights in the pursuit of the optimal healthcare journey.
In mid-2024, Arcadia acquired CareJourney, blending CareJourney’s clinically relevant cost, quality, and benchmark data into its next-generation healthcare data platform and workflow tools. Together,we put data to work at the speed, scale, and sophistication required to grow high-performing networks, accelerate digital transformation, and succeed in value-based care.
