Background
For countless individuals across the United States and the world, the outbreak of the COVID-19 pandemic prompted a rapid shift to digital life. In the healthcare industry, the sudden need to reduce patient travel and exposure while preserving provider capacity resulted in an unprecedented increase in the adoption of telemedicine. Within a matter of days, policymakers and payers expanded access to remote care, and providers and patients learned new technologies to ensure continuity of critical healthcare services.1,2
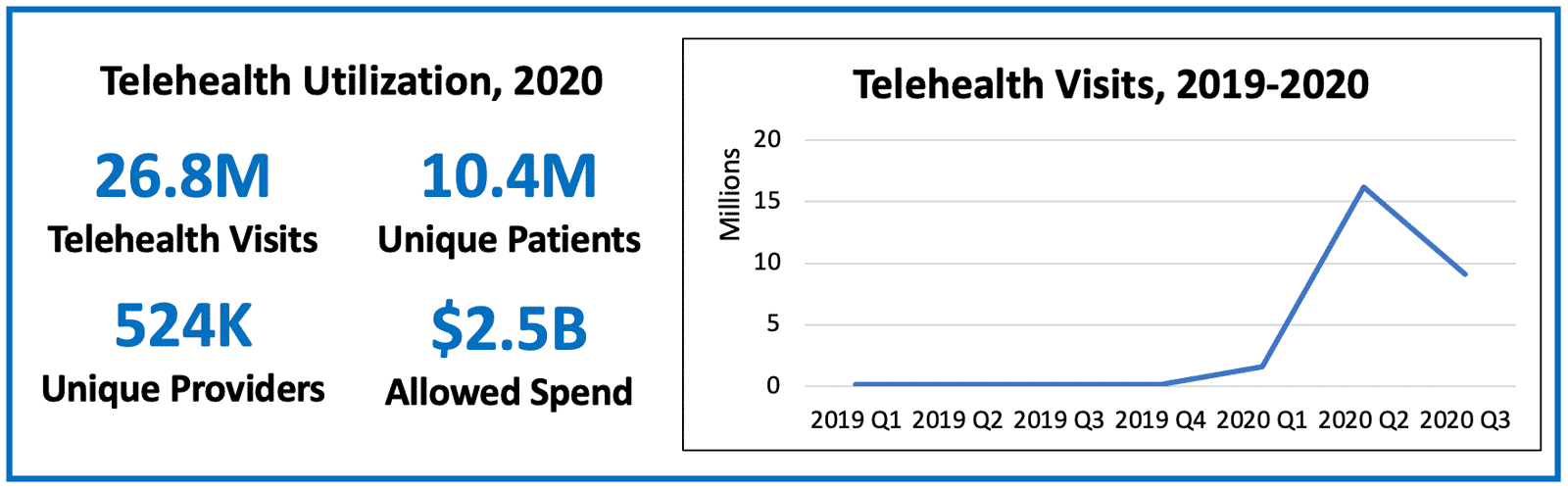
Figure based on national Medicare fee-for-service claims through September 2020 (claims runout through May 2020).
In response to the pandemic, the Centers for Medicare and Medicaid Services (CMS) provided CareJourney with access to up-to-date, national Medicare fee-for-service claims data. Building upon CareJourney’s existing data repository, this data access gives us the opportunity and responsibility to assist healthcare organizations in navigating changes in how care is delivered, which includes gaining a better understanding of how telehealth can be leveraged now and in the future.
Initial reports published by CMS in July found significant telehealth utilization through the beginning of the public health emergency (PHE), with nearly half (43.5%) of Medicare beneficiaries’ primary care visits provided via telehealth in April, and higher uptakes of telehealth among beneficiaries in initially harder-hit metropolitan areas.2,3
Three months after CMS’ initial report, CareJourney’s goal with this analysis is to:
- Further explore geographic variances in telehealth utilization
- Segment patient populations by key demographics to understand who has taken advantage of telemedicine thus far, and for whom future opportunities may exist
- Evaluate the persistence of telehealth adoption trends reported by CMS using additional months of data
The significant growth in telehealth claims data in 2020 enables us to gain an understanding of which geographies and patient populations have been best served by telehealth, and where additional room for growth exists.
What is Telehealth?
Telehealth is an umbrella term that typically encompasses the following types of telehealth:
- Synchronous virtual visits via video, telephone, or live chat
- Asynchronous chat-based interactions to enable communication and transmission of data between patients and providers
- The collection and transmission of health data from a non-clinical setting (such as a patient’s home) through remote patient monitoring
- Additional communication, education, monitoring, and care through technology-enabled modalities5
While the technologies enabling modern telemedicine are new and evolving, the concept of delivering medicine remotely is hardly new.6,7 Medicare first started covering telemedicine for patients in rural areas in 1999; however, significant restrictions resulted in limited utilization until the COVID-19 pandemic hit in early 2020.
2020 Telehealth Coverage & Policy Changes
In March, CMS announced that telehealth coverage was to be expanded for Medicare fee-for-service beneficiaries under Part B.8 This included several key updates:9
- For the duration of the public health emergency, telehealth visits are being considered the same as – and paid at the same rate as – in-person visits10
- Patients were previously required to connect to telehealth from a medical facility that had approved video conferencing technology;11 visits from home are now allowed via a personal digital device
- CMS loosened restrictions on the allowable technologies for telehealth visits, including those that are not HIPAA-compliant (such as FaceTime), for providers using them in good faith during the public health emergency
- Patients were previously required to have seen a provider face-to-face in the three years preceding a telehealth visit; that restriction has been waived to allow patients to see new providers and providers in other locations12
- The list of allowed services was expanded significantly, and multiple remote evaluation and management codes were added to the list of attribution-eligible primary care services for ACOs.13 This list of allowed services continues to be expanded, with 11 new codes added as recently as October 14.14
- In addition to expansions for Medicare fee-for-service beneficiaries, CMS offered greater flexibility to Medicare Advantage plans to offer telehealth services as well.15
The combination of these changes resulted in millions of patients and hundreds of thousands of providers utilizing telehealth that had not previously, as explored below.
Responding to Change: Analysis of Telehealth Adoption in 2020
Building upon CMS’ initial reports, CareJourney has leveraged the 100% Medicare fee-for-service claims database to begin exploring telehealth utilization for January through September of 2020.
In doing so, we seek to:
- Evaluate the variations in telehealth adoption among specific geographies, patient cohorts, and provider and care types
- Identify where telehealth has gained the most traction, and where additional room for growth exists
- Test initial hypotheses and establish the basis for further research question development in order to assess the lasting opportunities and impact of telehealth post-pandemic
How does telehealth utilization vary by geography?
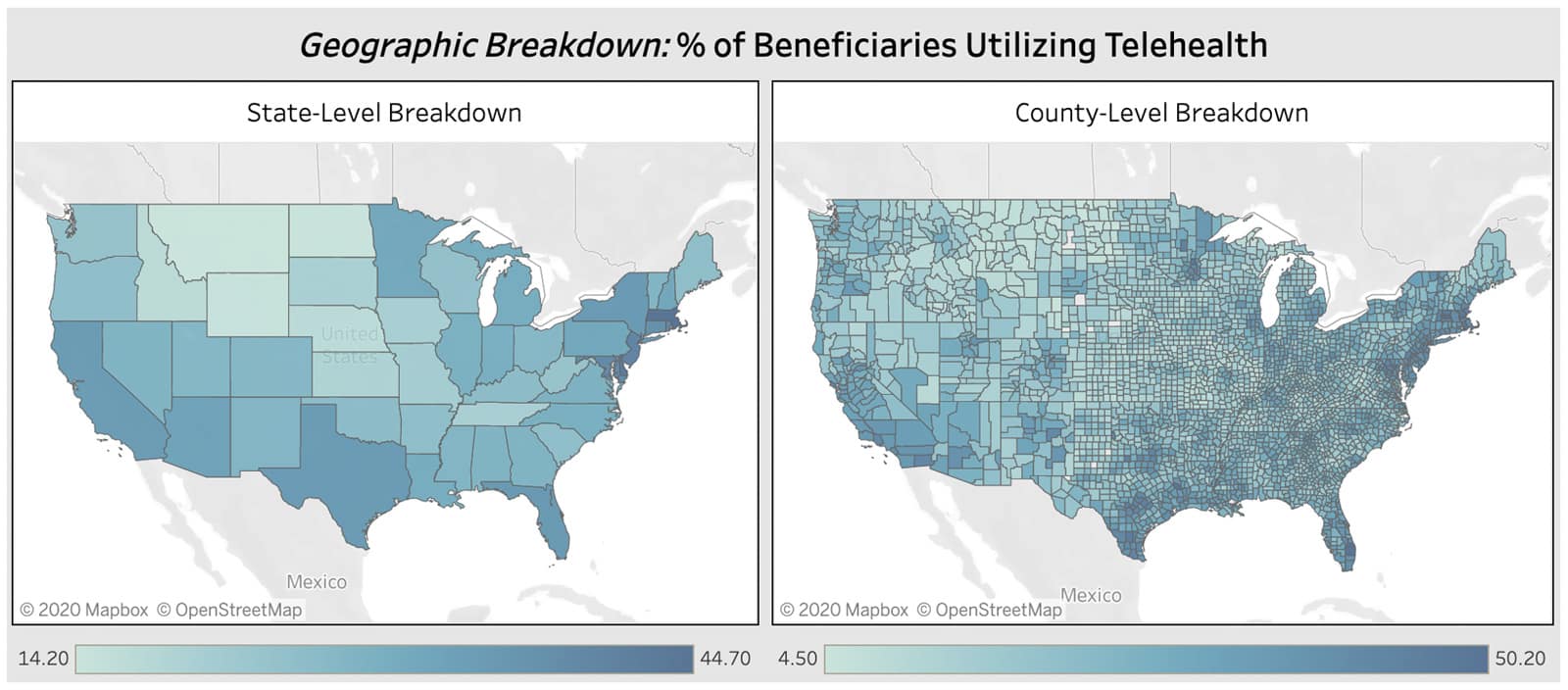
Nationwide, 30% of eligible Medicare beneficiaries had at least one telehealth visit in 2020, ranging from 14% adoption in Montana to 45% adoption in Massachusetts. Significant variation exists on a county-level as well, with Palm Beach County, Florida at the top with over 50% of resident Medicare patients having at least one telehealth visit.
Note that at the time of this analysis, claims runout was complete through May 2020, with September claims being the least complete, as providers have up to a year to submit claims.
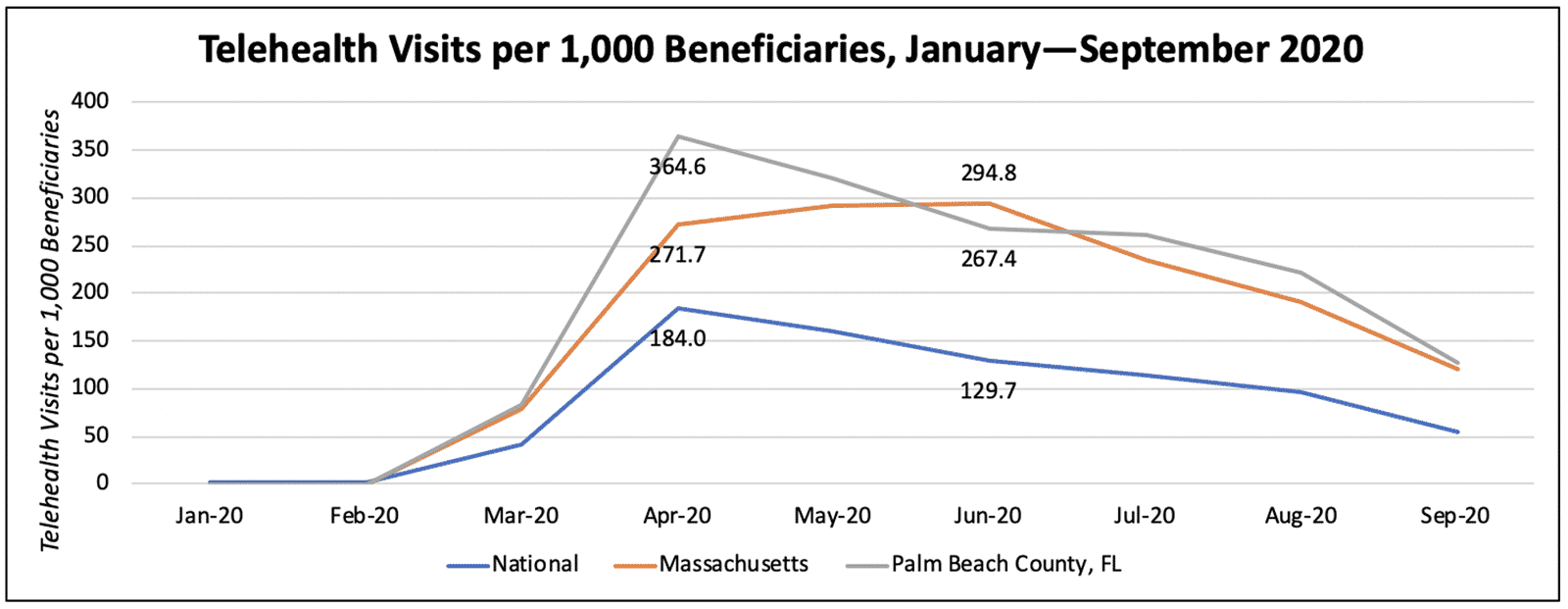
Looking month-over-month, we can see sustained but declining telehealth utilization at a national level. While Palm Beach County saw initially very high utilization (nearly 350 visits per 1,000 beneficiaries in April), an initial decline leveled out during the surge of COVID-19 cases in Florida in the summertime. Interestingly, the peak telehealth utilization in Massachusetts occurred in June, despite the fact that the Boston area was hardest hit at the beginning of the pandemic.
Who are the patients utilizing telemedicine?
Looking month-over-month, we can see sustained but declining telehealth utilization at a national level. While Palm Beach County saw initially very high utilization (nearly 350 visits per 1,000 beneficiaries in April), an initial decline leveled out during the surge of COVID-19 cases in Florida in the summertime. Interestingly, the peak telehealth utilization in Massachusetts occurred in June, despite the fact that the Boston area was hardest hit at the beginning of the pandemic.
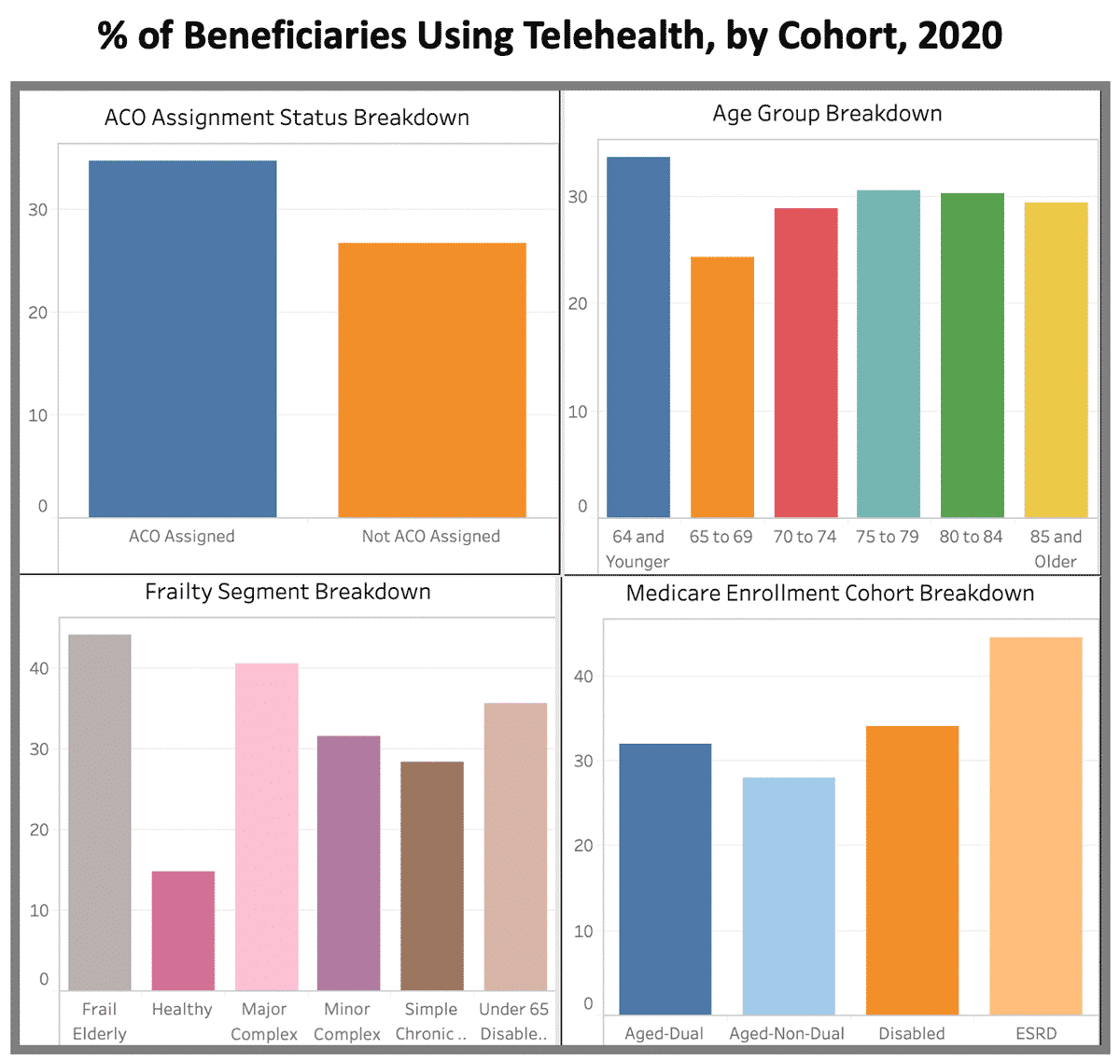
Looking at a patient cohort level nationwide, we see the following:
- ACO Assignment Status: ACO assigned beneficiaries are receiving care via telehealth at a higher rate than those not assigned to an ACO, both on the basis of adoption and visit volumes.
- Age Group: The adoption and visit rates among beneficiaries in the 70-74 through 85+ age groups are fairly consistent. One concern in treating older beneficiaries is potential discomfort in navigating the technology required to receive care via telehealth, but this does not appear to be a barrier for these beneficiaries more than any others. While younger aged beneficiaries (ages 65-69) are the lowest adopters and utilizers of telehealth, they are also likely among the healthiest. Beneficiaries under the age of 65 are the highest adopters of telehealth; however, these patients are generally enrolled in Medicare due to disability or ESRD status, and their care needs are often different than the general population of aged beneficiaries.
- Frailty Segment: Patients in the frail elderly and major complex chronic segments are the highest adopters of telehealth at 46% and 42% respectively. These are the patients for whom continuity of care was perhaps the most critical, and for whom it will be particularly important to research the long-term opportunities that telehealth presents.
- Medicare Enrollment Cohort: 36% of dual-eligible beneficiaries had used telehealth as of September 2020. This population requires further exploration, to evaluate how telemedicine could be leveraged in addressing adverse health outcomes driven by social determinants, and to understand where there are barriers to accessing virtual care that must be addressed.
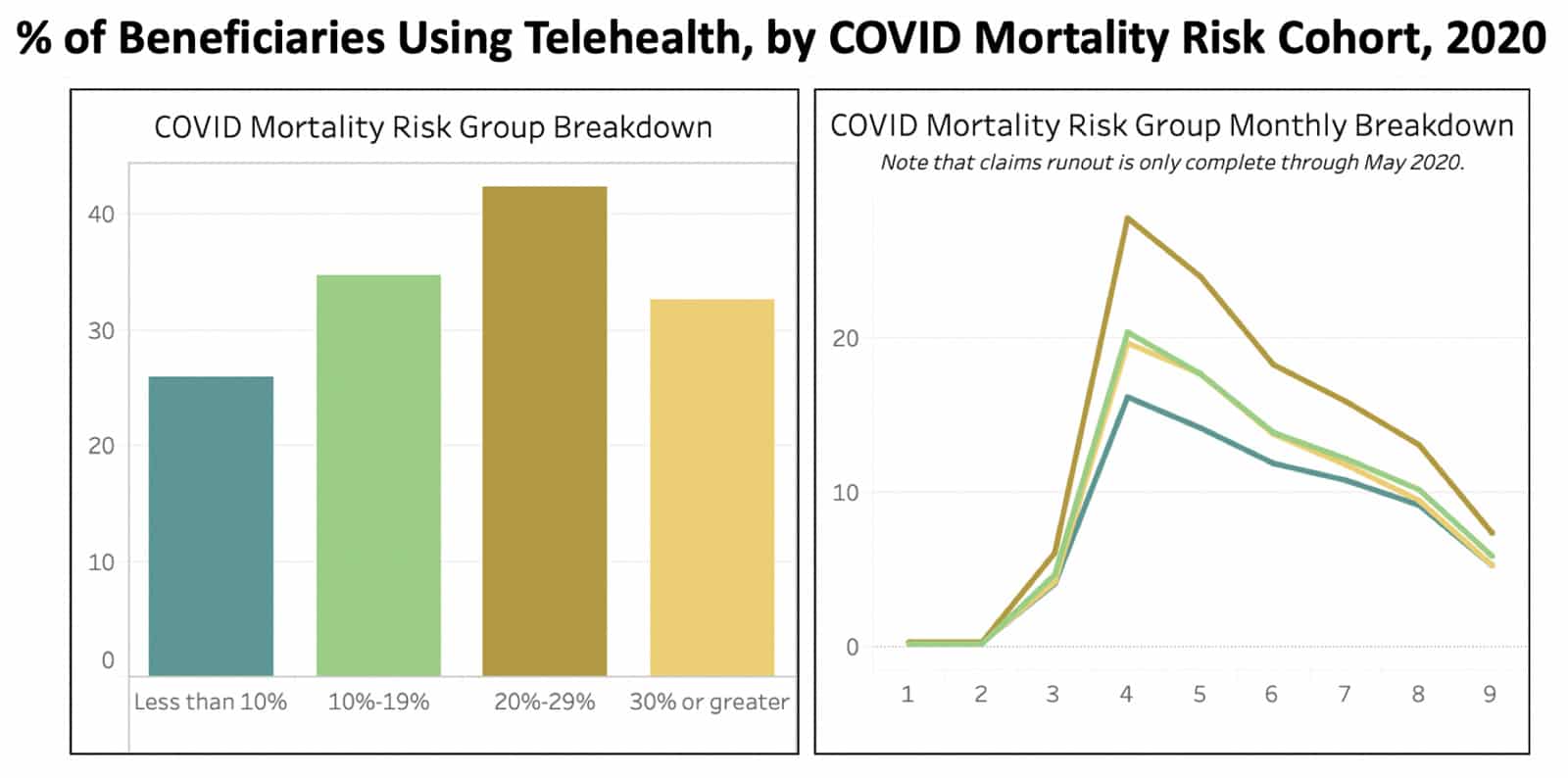
A newer patient segmentation methodology is the Predicted 30-Day COVID Mortality Model, developed through a collaboration between the U.S. Department of Veterans Affairs and the U.S. Department of Energy. This model segments patients based on patient age, gender, Charlson Comorbidity Index, and documented myocardial infarction (MI) or peripheral vascular disease (PVD), and assigns a percentage indicating the risk of death from COVID-19. Among these segments, patients in the second-highest mortality risk group were the highest adopters of telehealth, with 42% adoption overall, and 28% of those beneficiaries using telehealth in April alone. These patients have significant chronic conditions that required care continuity, similar to the groups discussed above.
Which providers are rendering telemedicine? What are they treating?
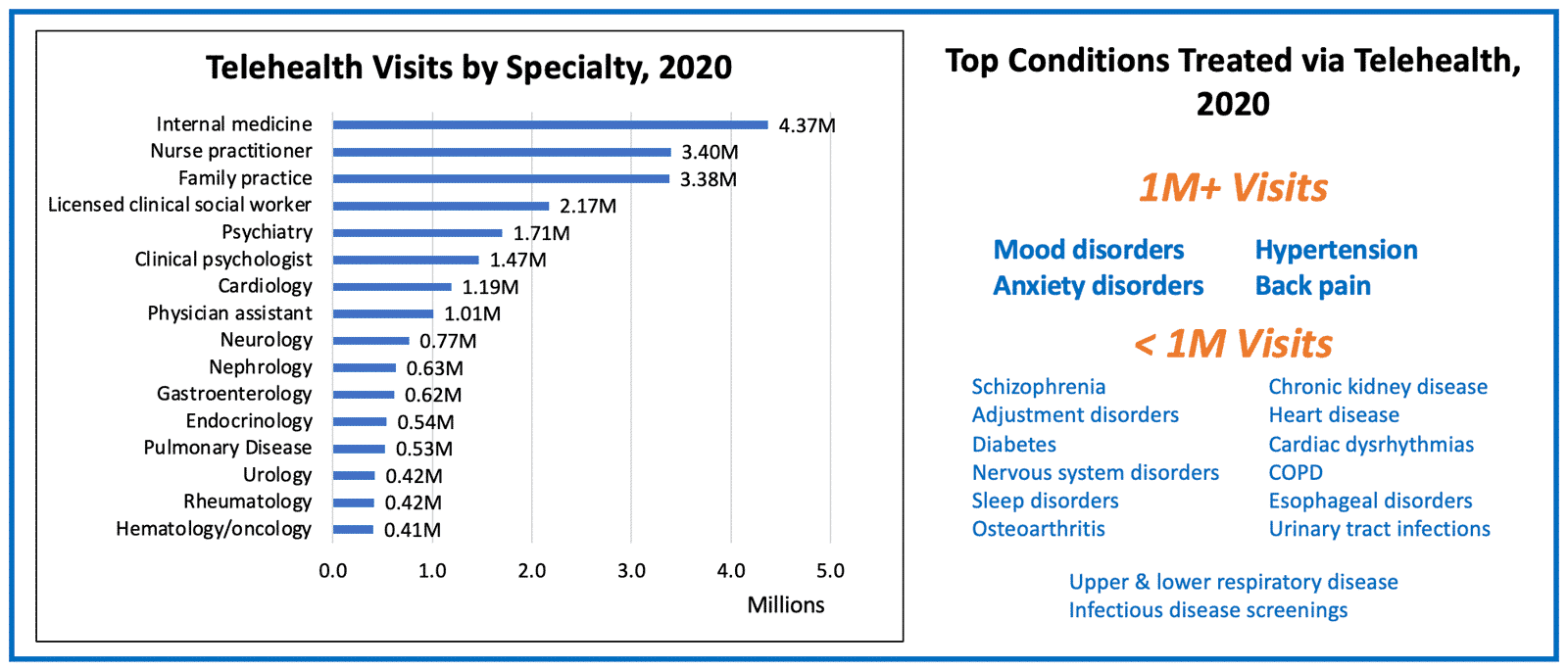
From a provider perspective, telehealth was used heavily among primary care providers and specialists to ensure the continuity of care for patients. Internal medicine and family practice providers saw nearly 8M visits, with common conditions like hypertension and back pain being frequently treated. Respiratory disease care and infectious disease screenings – likely for COVID-19 – were also among the top reasons for telehealth visits.
Management of chronic conditions accounted for millions of visits with providers across a diverse array of specialties, from cardiology to nephrology to endocrinology. Even among specialties with fewer virtual visits, like ophthalmology, providers are innovating on how to best capitalize on telehealth.16
The specialty area with the highest telehealth volume – and perhaps the highest potential for lasting telehealth utilization – is mental and behavioral health. Licensed clinical social workers, psychiatrists, and clinical psychologists rendered for over 5.4M telehealth visits, with mood disorders (e.g., depression) and anxiety disorders accounting for 3.3M and 1.6M visits respectively.
Looking to the Future: Lasting Impacts of Telehealth Expansion on Care Delivery
Post-pandemic, the ways in which telehealth utilization will persist remains to be seen. There are several points worth considering in understanding what the role of telehealth will be in the long-term for value-based care.
In what cases is telehealth most effective?
While there is some medicine that cannot be delivered remotely, telehealth may be particularly advantageous in areas such as chronic condition management and treatment of higher-touch or harder to reach individuals. The surge of telehealth may present new opportunities in post-acute management and at-home rehabilitation as well. Further comparative analysis is needed to better understand the impact of telehealth on health outcomes and total cost of care for specific conditions and patient cohorts.
How can telehealth provider quality be measured?
Current provider profiling methodologies (like CareJourney’s Provider Performance Index) focus on cost-effectiveness and patient outcomes over the duration of a period of care. Evaluating the impact of telehealth utilization throughout these episodes is key to understanding which providers are leveraging it effectively. While not all standard quality measures are applicable to telehealth, some, like diagnosis code capture, depression screening rates, and advanced care planning activities, can be tracked for providers across in-person and remote care settings for comparison.
Is telehealth working for patients?
In addition to claims-based assessment, patient feedback is critical in measuring and improving the quality of telehealth care. In September, the Agency for Healthcare Research and Quality (AHRQ) announced plans to release a telehealth patient experience survey, to better enable healthcare providers to understand patients’ expectations for and satisfaction with their telehealth care experiences. While this will not be officially considered part of the CAHPS suite of surveys before an extensive review, providers will be able to voluntarily submit data for benchmarking purposes.17
What are the barriers to lasting telehealth adoption?
It is important to consider that even with the regulatory barriers to telehealth significantly reduced, millions of Americans cannot access or afford the at-home broadband required to take advantage of it. Efforts are in place to mitigate this “digital divide”,18 including $200 million in Federal Communications Commission (FCC) funding appropriated through the CARES Act to help healthcare providers connect with patients via telehealth.19,20 Key issues of healthcare interoperability and privacy must also be addressed.
Conclusion: Is telehealth here to stay?
The COVID-19 pandemic forced the adoption of a new operating model in which telehealth took center stage. While there are numerous benefits to the expansion of telehealth, including improved access to care for vulnerable or hard-to-reach populations, cost and time efficiencies, and convenience,21 telehealth utilization among Medicare beneficiaries has already begun to wane in the months since stay-at-home orders began.
The 2021 Medicare physician fee schedule is currently under review,22and it is yet to be seen which of the changes will continue into the new year. For example, the equal reimbursement for in-person and virtual visits in 2020 made telehealth appealing; changing this could result in a significant reduction in providers’ willingness and ability to continue offering it. However, recent announcements from CMS indicate promising considerations regarding the future of telehealth access for Medicare beneficiaries.23,24
While the expansion of telehealth happened seemingly overnight, the long-term implementation of telehealth will require far more than just replacing in-person visits with virtual visits. Healthcare organizations must invest in strategic planning in order to understand the role and embrace the full potential of telehealth through the public health emergency and into the new normal.25,26
Telehealth Utilization Report
Explore with CareJourney
CareJourney looks forward to working with our membership in the coming months to continue navigating the topics raised in this blog post and taking advantage of the new and exciting volume of data to explore telehealth’s role in 2021 and beyond.
There are several ways in which CareJourney can further support healthcare organizations in harnessing the potential of telehealth in the pursuit of clinical excellence, including:
- Exploring and comparing actionable patient cohorts in terms of health status, demographics, and geography to understand who is best served by telehealth in terms of cost and outcomes
- Evaluating the markets that are strong adopters of telehealth as well as those markets which might benefit from a supplemental benefit offering to support the increased adoption of telehealth
- Identifying and profiling providers and practice groups rendering care via telehealth
- Investigating the downstream impacts of increased telehealth utilization for organizations in value-based agreements, such as on ACO or DCE attribution/alignment
- Advising on interoperability rules and standards for organizations navigating how to most effectively access and share patient information
If you are interested in understanding how CareJourney’s analytics can help with your organization’s telehealth strategy and care delivery, we want to hear from you! If you are currently a member, please reach out to your Member Services analyst for more information. If you’re not a CareJourney member, email us at jumpstart@carejourney.com, or you can learn more by requesting a meeting below.
- Abelson, R. (2020, March 11). Doctors and Patients Turn to Telemedicine in the Coronavirus Outbreak. The New York Times. Retrieved from https://www.nytimes.com/2020/03/11/health/telemedicine-coronavirus.html
- Mueller, B. (2020, April 4). Telemedicine Arrives in the U.K.: ‘10 Years of Change in One Week’. The New York Times. Retrieved from https://www.nytimes.com/2020/04/04/world/europe/telemedicine-uk-coronavirus.html
- U.S. Department of Health & Human Services ASPE. (2020, July 28). ASPE Issue Brief: Medicare Beneficiary Use of Telehealth Visits: Early Data From the Start of the COVID-19 Pandemic. Retrieved from https://aspe.hhs.gov/pdf-report/medicare-beneficiary-use-telehealth
- Verma, S. (2020, July 15). Early Impact Of CMS Expansion Of Medicare Telehealth During COVID-19. Health Affairs. Retrieved from https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/
- American Telemedicine Association. Telehealth: Defining 21st Century Care. Retrieved from https://www.americantelemed.org/resource/why-telemedicine/
- Novak, M. (2012, March 14). Telemedicine Predicted in 1925. Smithsonian Magazine. Retrieved from https://www.smithsonianmag.com/history/telemedicine-predicted-in-1925-124140942/
- Iafolla, T. (2016). History of Telemedicine Infographic. Retrieved from https://blog.evisit.com/virtual-care-blog/history-telemedicine-infographic
- Centers for Medicare & Medicaid Services. (2020, September 11). COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing. Retrieved from https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf (Page 59)
- U.S. Department of Health & Human Services ASPE. (2020, July 28). ASPE Issue Brief: Medicare Beneficiary Use of Telehealth Visits: Early Data From the Start of the COVID-19 Pandemic. Retrieved from https://aspe.hhs.gov/pdf-report/medicare-beneficiary-use-telehealth (Page 11)
- Centers for Medicare & Medicaid Services. (2020, March 17). Medicare Telemedicine Health Care Provider Fact Sheet. Retrieved from https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- Quinn, W. (2019, August). Telehealth and Medicare: What Is Covered. Retrieved from https://www.aarp.org/content/dam/aarp/ppi/2019/08/telehealth-medicare-what-is-covered.doi.10.26419-2Fppi.00080.001.pdf
- Miller, M. (2020, March 24). Medicare Is Updating Coverage to Help in the Coronavirus Crisis. The New York Times. Retrieved from https://www.nytimes.com/2020/03/24/business/coronavirus-medicare-elderly.html?referringSource=articleShare%203/5
- Centers for Medicare & Medicaid Services. (2020, April 29). Medicare Shared Savings Program: CMS Flexibilities to Fight COVID-19. Retrieved from https://www.cms.gov/files/document/covid-ifc-2-medicare-shared-savings-program.pdf (Page 3)
- Centers for Medicare & Medicaid Services (2020, October 14). Trump Administration Drives Telehealth Services in Medicaid and Medicare. Retrieved from https://www.cms.gov/newsroom/press-releases/trump-administration-drives-telehealth-services-medicaid-and-medicare
- Minemyer, P. (2020, May 22). CMS finalizes plan to allow Medicare Advantage plans to expand telehealth benefits. Retrieved from https://www.fiercehealthcare.com/payer/cms-finalizes-plan-to-allow-medicare-advantage-plans-to-expand-telehealth-benefits
- ASCRS. (2020). CMS Expands Medicare Telehealth Benefits During COVID-19 Public Health Emergency. Retrieved from https://ascrs.org/advocacy/regulatory/telemedicine
- Castellucci, M. (2020, September 24). AHRQ plans to release a telehealth patient experience survey. Modern Healthcare. Retrieved from https://www.modernhealthcare.com/technology/ahrq-plans-release-telehealth-patient-experience-survey
- Starks, G. (2020, March 19). To Fight Coronavirus, Millions More Americans Need Internet Access. The New York Times. Retrieved from https://www.nytimes.com/2020/03/19/opinion/internet-broadband-coronavirus.html
- Federal Communications Commission. (2020, September 28). COVID-19 Telehealth Program. Retrieved from https://www.fcc.gov/covid-19-telehealth-program
- Alliance for Connected Care. (2020, March 27). Telehealth in the Third COVID Legislative Package. Retrieved from http://connectwithcare.org/telehealth-in-the-third-covid-legislative-package/
- American Telemedicine Association. Telehealth: Defining 21st Century Care. Retrieved from https://www.americantelemed.org/resource/why-telemedicine/
- Centers for Medicare & Medicaid Services. (2020, August 4). Physician Fee Schedule. Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched
- Centers for Medicare & Medicaid Services. (2020, August 3). Trump Administration Proposes to Expand Telehealth Benefits Permanently for Medicare Beneficiaries Beyond the COVID-19 Public Health Emergency and Advances Access to Care in Rural Areas. Retrieved from https://www.cms.gov/newsroom/press-releases/trump-administration-proposes-expand-telehealth-benefits-permanently-medicare-beneficiaries-beyond
- Minemyer, P. (2020, September 1). Verma: CMS will mull which COVID-19 flexibilities may stick around post-pandemic. Retrieved from https://www.fiercehealthcare.com/payer/verma-cms-will-mull-which-covid-19-flexibilities-may-stick-around-post-pandemic
- Bestsennyy, O., Gilbert, G., Harris, A., & Rost, J. (2020, June 1). Telehealth: A quarter-trillion-dollar post-COVID-19 reality? Retrieved from https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality
- Woods, R. (2020, July 1). You promised a telehealth revolution after Covid-19. Don’t backslide now. Retrieved from https://www.advisory.com/research/physician-executive-council/prescription-for-change/2020/06/telehealth